| Share |  |
 | |||
Exploring the Cholesterol Myth
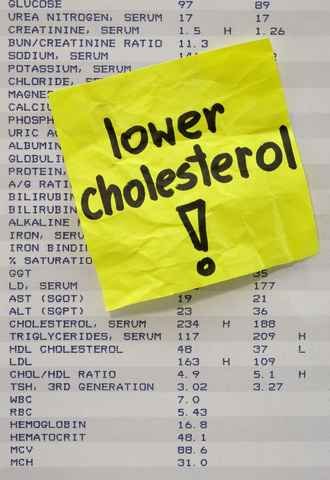 If you live in this society and are exposed to media to any degree, you have undoubtedly been warned time and again about cholesterol and the need to prevent its build-up in your arteries. Repeatedly hearing these commercial messages makes most people want to do whatever they can to avoid getting clogged arteries, especially when it could mean a heart attack that might be fatal.
If you live in this society and are exposed to media to any degree, you have undoubtedly been warned time and again about cholesterol and the need to prevent its build-up in your arteries. Repeatedly hearing these commercial messages makes most people want to do whatever they can to avoid getting clogged arteries, especially when it could mean a heart attack that might be fatal.
Cholesterol and heart disease have been inextricably linked for the last half-century. But in spite of all the push for low-fat diets and the growing use of cholesterol-lowering drugs, the death rate from heart disease has not decreased to any measurable degree. Contrary to popular belief, results of many hundreds of documented scientific studies show little relationship between high cholesterol levels and increased incidences of heart attacks or deaths from coronary heart disease. In fact, results from one of the largest and longest running studies showed that half of the participants with heart disease had low cholesterol, and half of the people without heart disease had high cholesterol.
Considering this type of information is not so widely promulgated through the media, the majority of people are unaware of the latest research about the true causes of heart disease. But if you examine the evidence, you just might conclude that perhaps cho lesterol is not quite the “culprit” it is made out to be. You may even gain an appreciation of the fact that God created it for a number of valuable purposes vital to our health.
lesterol is not quite the “culprit” it is made out to be. You may even gain an appreciation of the fact that God created it for a number of valuable purposes vital to our health.
What is Cholesterol?
Although both fats and cholesterol are termed “lipids” (molecules that are fat-soluble), cholesterol is actually a sterol (special type of lipid), and not a fat. Because fat-soluble substances cannot dissolve in the water-based blood stream, they must be carried inside of water-soluble molecular complexes called lipoproteins, which ar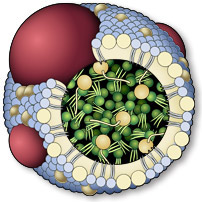 e mixtures of triglycerides, phospholipids, cholesterol and protein. The body binds fats to proteins to form these compounds. High-density lipoproteins (HDL) consist of approximately 50% protein with most of the lipid portion consisting of triglycerides (which are water-soluble compounds composed of three fatty acids combined with glycerol). Low-density lipoproteins (LDL) have more cholesterol than triglycerides and are lower in protein. VLDL (very low density lipoprotein) is a third type of lipoprotein made primarily in the liver, which converts to LDL through triglyceride loss. The ratio of HDL to LDL is constantly adjusted to meet the body’s needs at any given time.
e mixtures of triglycerides, phospholipids, cholesterol and protein. The body binds fats to proteins to form these compounds. High-density lipoproteins (HDL) consist of approximately 50% protein with most of the lipid portion consisting of triglycerides (which are water-soluble compounds composed of three fatty acids combined with glycerol). Low-density lipoproteins (LDL) have more cholesterol than triglycerides and are lower in protein. VLDL (very low density lipoprotein) is a third type of lipoprotein made primarily in the liver, which converts to LDL through triglyceride loss. The ratio of HDL to LDL is constantly adjusted to meet the body’s needs at any given time.
People often regard HDL as the “good” cholesterol and LDL as the “bad” cholesterol but the truth is that it is the same cholesterol in both of them. Both types of lipoproteins serve important functions in the body. Neither is “bad,” although small dense particles of LDL may create inflammation in the lining of arteries if they become oxidized and turn rancid . However, why that occurs is a separate matter unrelated to cholesterol, as I will explain in next month’s article. The job of LDL is to transport manufactured cholesterol from the liver to the tissues of the body. HDL’s role is to take cholesterol back to the liver where it is recycled and placed into other particles for transport to tissue and cells. If cholesterol were “bad,” HDL would take it to the kidneys or the intestines for elimination instead.
. However, why that occurs is a separate matter unrelated to cholesterol, as I will explain in next month’s article. The job of LDL is to transport manufactured cholesterol from the liver to the tissues of the body. HDL’s role is to take cholesterol back to the liver where it is recycled and placed into other particles for transport to tissue and cells. If cholesterol were “bad,” HDL would take it to the kidneys or the intestines for elimination instead.
Redeeming Cholesterol’s Reputation
The value of cholesterol cannot be overstated, as good health is not possible without adequate amounts of it in the body. Cholesterol is needed for:
- Maintaining the structure of cells – cholesterol acts like “superglue” to hold together the lipid cell layers which give cell walls their strength.
- Production of bile salts - needed for the breakdown and digestion of fat and to facilitate the absorption of fat-soluble vitamins (A, D, E and K) and minerals. Approximately 60-80 percent of cholesterol is used to form cholic acid for the production of bile salts.
- Adequate production of adrenal and reproductive hormones - cholesterol is the basic building block for cortisol, aldosterone, progesterone, estrogen, testosterone, pregnenolone, and DHEA. A balanced hormonal system is necessary for achieving and maintaining optimal health.
- Synthesis of vitamin D - produced as UVB rays from the sun come in contact with cholesterol contained on our skin. Vitamin D is vital for the bones and nervous system, proper growth, mineral metabolism, muscle tone, insulin production, reproduction, and immune system function.
- Good brain and neurological function – cholesterol is the primary organic molecule in the brain and is needed for the myelin sheath that covers all of our nerve cells.
- Healthy immune function – higher levels of cholesterol provide greater amounts of immune cells to fight infection.
- Protection against environmental toxins (heavy metals, xenoestrogens, pesticides, halogens, etc.) Cholesterol helps to bind toxins and protect brain and nerve tissue from chemical damage.
- Skin protection – cholesterol makes skin water tight and impermeable to various substances that would try to penetrate it and prevents water loss.
- Repair and healing – the liver produces large amounts of cholesterol when there is damage to the cells and tissue of the body.
Flawed Theories
If God created cholesterol for so many good purposes in our bodies, how did it get blamed for heart disease? In order to understand why this occurred, it may be helpful to know a little background on how some of these theories developed and gained wide acceptance among the scientific community and, hence, the general publi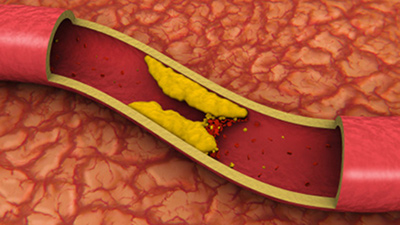 c. For most of the last 50 years, low-fat foods, food pyramids with strict limits on dietary fat, drugs that block fat absorption and cholesterol synthesis, and other measures to combat “fat” in people’s arteries and bodies have been the trend. Steering clear of diets too high in saturated fats and cholesterol has been considered the key to the prevention and treatment of coronary heart disease. In spite of all these efforts to decrease fat, heart disease remains the leading cause of death while obesity and diabetes have nearly doubled. It doesn’t seem to be working.
c. For most of the last 50 years, low-fat foods, food pyramids with strict limits on dietary fat, drugs that block fat absorption and cholesterol synthesis, and other measures to combat “fat” in people’s arteries and bodies have been the trend. Steering clear of diets too high in saturated fats and cholesterol has been considered the key to the prevention and treatment of coronary heart disease. In spite of all these efforts to decrease fat, heart disease remains the leading cause of death while obesity and diabetes have nearly doubled. It doesn’t seem to be working.
In the 1870’s, a German pathologist by the name of Rudolph Virchow found that plaque in the arteries of patients who had died contained significant amounts of cholesterol. He conceived the theory that cholesterol infiltrated the walls of the arteries from the blood. This theory came to be known as the “Lipid Hypothesis,” which eventually evolved into the “Cholesterol Theory” of today. In 1925, it was first discovered that the body manufactured several times more cholesterol than was consumed in the diet. Although the “Lipid Hypothesis” was questioned to some extent at that time, the majority of researchers continued to pursue the theory that fat in the diet was the primary cause of heart disease. The following statements comprise the basic premises of the “Cholesterol Theory.”
- Heart attacks are caused by a buildup of cholesterol plaques inside the coronary arteries.
- Cholesterol plaques are caused by an elevated level of cholesterol in the blood.
- A high-fat, high-cholesterol diet will raise the blood cholesterol level and thus put a person at risk for coronary artery disease, eventually leading to heart attack and, likely, premature death.
- Lowering the cholesterol level with diet and/or drugs will decrease the risk of developing coronary artery disease, prevent heart attacks, and save countless lives.
Although the Cholesterol Theory o riginated with well-intentioned researchers who set out to identify “risk factors” for coronary heart disease, it seemed initial research was interpreted through the lens of popular theories about fat and cholesterol at the time. Ancel Keys, a doctor of physiology, conducted one of the first published studies in 1953. Dr Keys set out to prove what he considered the direct relationship between increased intake of fat and increased mortality from heart disease. He did so by compiling data from 22 countries based on two factors - the percentage of dietary fat and the death rate from coronary heart disease. The problem was that he only included countries that fit his hypothesis in his published analysis. In six of the western countries he chose, there seemed to be a direct correlation between dietary fat and mortality from heart disease. The other sixteen countries were omitted, as there was no such clear-cut correlation. This study is still regarded as support for the “cholesterol=heart disease” hypothesis found in medical textbooks and within the medical community.
riginated with well-intentioned researchers who set out to identify “risk factors” for coronary heart disease, it seemed initial research was interpreted through the lens of popular theories about fat and cholesterol at the time. Ancel Keys, a doctor of physiology, conducted one of the first published studies in 1953. Dr Keys set out to prove what he considered the direct relationship between increased intake of fat and increased mortality from heart disease. He did so by compiling data from 22 countries based on two factors - the percentage of dietary fat and the death rate from coronary heart disease. The problem was that he only included countries that fit his hypothesis in his published analysis. In six of the western countries he chose, there seemed to be a direct correlation between dietary fat and mortality from heart disease. The other sixteen countries were omitted, as there was no such clear-cut correlation. This study is still regarded as support for the “cholesterol=heart disease” hypothesis found in medical textbooks and within the medical community.
Evidence that scientifically refutes each of the tenets of the Cholesterol Theory has existed for decades but has not received the same media attention as those endorsed by organization like the American Heart Association or the National Heart, Lung and Blood Institute (part of the National Institutes of Health). As an example, many studies and experiments have been conducted in which humans were either given five to ten times more dietary cholesterol than normal or had cholesterol virtually removed from their diet altogether. In both instances, though an initial rise or drop in levels may have occurred, cholesterol levels always returned to near normal levels. The bottom line is that the amount of cholesterol that one eats plays a very minor role in determining cholesterol levels.
A Cardiologist’s Search for Answers
While completing his postgraduate cardiology fellowship at a large community hospital, Dr. Ernest Curtis, author of The Cholesterol Delusion, observed hundreds of patients who suffered from coronary heart disease and did not fit the “risk factor” profile he had been taught. That motivated him to engage in intensive independent study of over 500 medical journal articles and reviews on the topics of diet, cholesterol, and coronary artery disease. As he examined t he references cited by the articles, he noticed that they all led back to the original studies upon which the Cholesterol Theory was based.
he references cited by the articles, he noticed that they all led back to the original studies upon which the Cholesterol Theory was based.
Most people are surprised to learn that diet has little direct effect on blood cholesterol levels (though it may greatly contribute to the underlying root cause of heart disease). Even more surprising is that there is no debate concerning this fact among knowledgeable scientists. From all of his research, Dr. Curtis concluded that no sound scientific evidence exists to support any of the premises of the Cholesterol Theory. In other words, what causes the development of atherosclerosis and coronary heart disease is neither cholesterol levels nor fat in the diet. Dr. Curtis challenges everyone to examine the evidence cited by the proponents of the Cholesterol Theory to see if it stands up to critical examination. In the appendixes of the book, he includes the medical journal articles reporting on the two clinical trials most often cited today as proof of the cholesterol theory (the Lipid Research Clinics Trial and the Helsinki Heart Study). Since it would be too lengthy for me to sufficiently expound on the details and evidence for his conclusions within the scope of this article, I would highly recommend that anyone interested in understanding more about the facts pertaining to the relationship of cholesterol and heart disease read The Cholesterol Delusion. In addition, Dr. Uffe Ravnskov’s book Fat and Cholesterol are Good for You goes into detailed analysis concerning misinformation found in the major studies commonly used to support this theory.
Risks Associated with Low Cholesterol Levels
The majority of people are not aware that cholesterol levels which are too low present greater risks to health than high cholesterol levels. Listed below are examples of adverse effects created by low cholesterol levels along with a few of the numerous (over 900) studies that lend credence to this premise.
Cancer
An increase in cancer is clearly linked with low cholesterol levels. Numerous studies support findings that reveal a high risk of cancer in people whose cholesterol levels are less than 160, with the highest risk associated with those whose levels were 140 or less. An increased risk of cancer is linked with cholesterol levels less than 190 and an average risk is found in people whose levels are between 195 and 210. The lowest risk for cancer occurs when cholesterol levels are above 240.
In a study conducted by a medical institute in Paris, France involving 6,230 working men, age 43-52, participants whose total cholesterol dropped the most from a mean baseline level of 222 were approximately 25% more likely to die from cancer. The cholesterol levels of the men w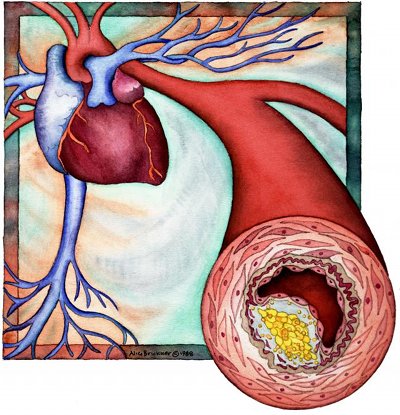 ere recorded several times a year as they were followed over the course of 17 years. One of the longest running studies on cholesterol levels (the Framingham study) revealed that the chances of dying from cancer doubled if cholesterol levels dropped significantly over a four-year period. Another study conducted in Japan with nearly 50,000 patients treated with the statin drug Zocor for five years concluded that death from cancer was three times higher in the group whose cholesterol was reduced the most compared to other groups in which cholesterol was not lowered as significantly
ere recorded several times a year as they were followed over the course of 17 years. One of the longest running studies on cholesterol levels (the Framingham study) revealed that the chances of dying from cancer doubled if cholesterol levels dropped significantly over a four-year period. Another study conducted in Japan with nearly 50,000 patients treated with the statin drug Zocor for five years concluded that death from cancer was three times higher in the group whose cholesterol was reduced the most compared to other groups in which cholesterol was not lowered as significantly
Heart Disease
The rate of deaths from heart disease has not decreased in spite of measures taken to lower cholesterol through diet or cholesterol-lowering drugs over the last 50 years. Not only does lowering cholesterol fail to decrease the risk of heart disease but it also greatly increases the chance of dying from a heart attack when one occurs. At least half of heart attack victims have cholesterol readings in the low or normal range. Listed below are a few examples of various studies that refute the validity of the theory that low cholesterol decreases the risk of heart disease.
- The cholesterol levels of 137,000 heart patients admitted to 541 hospitals because of acute heart attacks were measured within 24 hours of admission. Both total cholesterol and LDL cholesterol were lower than normal when compared with the average (this study was conducted by the medical department of the University of California).
- A study of cholesterol levels in over 4,000 men and woman 75 and above showed that those with total cholesterol levels less than 160 had the highest rate of death from coronary disease whereas the risk for death was lower in those whose total cholesterol levels were greater than 240.
- An analysis of 1,134 patients with heart disease showed that elevated cholesterol was not associated with hypertension, diabetes or coronary heart disease but that the chance of dying from a heart attack was greater in those with low cholesterol (Journal of Cardiac Failure).
- A Japanese study found that death rates from chronic heart disease went down as cholesterol levels went up.
Increased Mortality
Studies also support the fact that “all cause mortality” (death from any cause) is linked to low cholesterol levels.
- In a study of 11,500 patients published in the European Heart Journal, the ones with low cholesterol had twice the risk of death than those with high cholesterol.
- A study from the University of Innsbruck in Austria of 150,000 people showed that low cholesterol levels were a predictor of premature death in men of all ages as well as woman over the age of 50.
- In a study with elderly females, the death rate was 5.2 percent higher in those whose cholesterol levels were under 155 (the elderly are particularly sensitive to lowered cholesterol levels).
Immune Dysfunction
Individuals with low cholesterol suffer more with frequent and severe infections than the average population. Studies have shown that people with lowered cholesterol levels have fewer circulating lymphocytes, total T-cells and helper T-cells as compared to those with higher cholesterol levels.
Brain and Neurological Impairment
Depression, increased risk of suicide, violent behavior and aggression, impaired memory and mental focus, Parkinson’s and other neurological diseases all are associated with low cholesterol levels. Reduced brain serotonin activity is thought to account for some of these effects.
Reduced Protection from Neurotoxins, Mercury and Heavy Metals
The body is exposed to even more inflammation and free radical damage since less cholesterol is available to bind with toxins
Statin Drugs to the Rescue?
In spite of the fact that results from more and more studies confirm just how unhealthy lowering cholesterol is to the body, more prescriptions for cholesterol-lowering drugs are given to Americans today than ever before. In fact, statin drugs are the most prescribed drug in the country, representing a 30 billion dollar market. There is no doubt that these drugs effectively lower cholesterol levels. But is just lowering cholesterol addressing the real cause of heart disease? I would suggest that it is more a means of masking a symptom rather than dealing with the true underlying cause as I will cover further in next month’s health article.
more and more studies confirm just how unhealthy lowering cholesterol is to the body, more prescriptions for cholesterol-lowering drugs are given to Americans today than ever before. In fact, statin drugs are the most prescribed drug in the country, representing a 30 billion dollar market. There is no doubt that these drugs effectively lower cholesterol levels. But is just lowering cholesterol addressing the real cause of heart disease? I would suggest that it is more a means of masking a symptom rather than dealing with the true underlying cause as I will cover further in next month’s health article.
The way statin drugs work is to impede the manufacturing of cholesterol in the liver by poisoning a crucial enzyme involved in that process. There are clear consequences that occur as a result of interfering with a biochemical pathway of the body. As Dr. David Brownstein often states, “you can’t poison an enzyme or block an important receptor in the body for the long-term and expect a good outcome.” In addition to increased risk of cancer (covered in the preceding section), statin drugs may cause any of the following side effects:
Depleted CoQ10 Production
 Statin drugs block the production of CoQ10, a vital nutrient needed by the body for energy and cardiovascular health. CoQ10 production decreases proportionately with cholesterol since they are both produced in the same pathway affected by the poisoned enzyme. Lowering the production of CoQ10 leads to a loss of cell energy and increased free radical damage, which damages the mitochondrial DNA and accelerates aging and degeneration in the body.
Statin drugs block the production of CoQ10, a vital nutrient needed by the body for energy and cardiovascular health. CoQ10 production decreases proportionately with cholesterol since they are both produced in the same pathway affected by the poisoned enzyme. Lowering the production of CoQ10 leads to a loss of cell energy and increased free radical damage, which damages the mitochondrial DNA and accelerates aging and degeneration in the body.
Since CoQ10 is vital for maintaining optimal muscle function, this especially impacts the heart since it is the largest muscle with the highest concentrations of CoQ10. Karl Folkers, the American biochemist who discovered the molecular structure of CoQ10, found that heart function deteriorated with decreased concentrations of CoQ10 from the use of a statin drug. However, when individuals were given CoQ10, their heart recovered. Numerous controlled studies on heart disease demonstrate the effectiveness of CoQ10 for improving heart muscle function and repairing heart damage. CoQ10 is also useful for maintaining good cognitive function. It is vital that anyone taking a statin drug also take a CoQ10 supplement. Unfortunately, not every physician informs their patients about the reality of CoQ10 depletion with the use of statin drugs or of the need for supplementation.
Increased Risk of Heart Failure
In a study conducted in December of 2008 involving 17,791 hospitalized heart failure patients, it was discovered that the higher the cholesterol levels, the lower the death rate. The use of statin drugs in this study was associated with a higher rate of cardiovascular death. Studies have shown that for every one-point reduction in total cholesterol per year, cardiovascular death rates increased 14%. Although no corresponding decline in the thickness of arteries is linked with the use of statin drugs, increased thickness has been observed. In addition, the use of statin drugs appears to make C-reactive protein and homocysteine test results worst. Both of these are key markers that indicate the risk of heart disease.
Brain Fog and Dementia
Proper brain function cannot occur without adequate cholesterol levels since most of the brain is composed of fats. A steady production of cholesterol is needed for the creation of nerve impulses. Neuropathic damage and cognitive dysfunction with memory loss are reported with statin drug use.
Liver or Muscle Damage
Because severe liver damage can occur with statin drug use, frequent blood tests must be taken to check for liver enzyme when individuals take them. Muscle pain and weakness is one of the most common side effects. This should be of no surprise since CoQ10 is necessary for optimal muscle function. If statin-produced muscle pain continues, it can result in a form of muscle damage known as rhabdomyolysis, in which large amounts of a protein present within muscle cells are released into the blood stream where they can affect, and, potentially cause permanent damage to the kidneys.
Immune Depression
According to the Alliance for Natural Health, statin drugs can hinder the ability of the body’s immune cells to kill pathogens. Research conducted in Switzerland showed that certain statin drugs suppress the helper T-cells, a type of immune cell that recognizes foreign pathogens and activates the appropriate T-cells and B-cells to respond (suppressed helper T-cells also occurs with AIDS).
Hormone Imbalance
Erectile dysfunction, low libido and infertility are among the side effects reported from decreasing the precursor substance from which hormones are produced.
Other Side Effects
Typical drug side effects like upset stomach, headache, skin rash, dizziness, weakness and fatigue are also common with the use of statin drugs. Other side effects include difficulty sleeping, peripheral neuropathy (14x greater risk), pancreas dysfunction (raised insulin levels), and cataracts.
What About the Positive Studies on Statins?
The National Cholesterol Education Program was organized in 1985 to educate professionals and the public about the benefits of lowering cholesterol levels to reduce the risk of coronary heart disease. To support the commonly accepted hypothesis (reduced cholesterol equals reduced heart disease risk),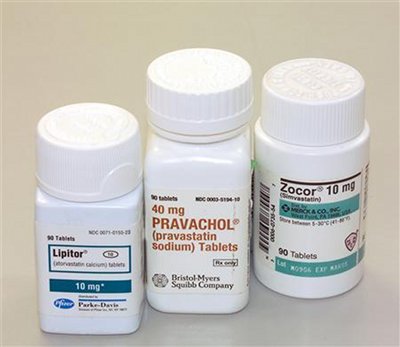 they issued what was described as an “evidence-based” set of guidelines on cholesterol management in 2001. Since that time, five major clinical trials using statin therapy have been published that are cited as support for the theory that lowering cholesterol levels results in a lower risk of heart disease.
they issued what was described as an “evidence-based” set of guidelines on cholesterol management in 2001. Since that time, five major clinical trials using statin therapy have been published that are cited as support for the theory that lowering cholesterol levels results in a lower risk of heart disease.
In four of the five trials (the fifth trial was comparing two different statin drugs), two groups of people were followed for a set length of time – one group received a statin drug and the other group received a placebo. The studies ranged in length from 3.3 years to 6 years. Among the 56,037 people studied, there was only a 0.775% advantage with regard to mortality rates (based on the number of people who remained alive at the conclusion of the study in both groups). In one of the studies, there was a significant increase in cancer in the group who took the statin drug.
Considering that there are much safer ways to lower your risk of heart disease than taking statin drugs, it would seem that a reduction of only 0.775% is hardly worth chancing the possible damaging side effects of these drugs. The associated risk of using statin drugs far outweighs evidence based on a study with statistically insignificant results.
The JUPITER study, published in the New England Journal of Medicine in 2008, was the most recent study to make headlines when it announced that the statin drug Crestor could even cut the risks of heart attacks in healthy patients. This study boasted that statin drugs could lower the risk of heart attack by 54%, the risk of stroke by 48%, the risk of needing angioplasty or bypass surgery by 46%, and the risk of death fr om all causes by 20%. Careful review of the methods and results of the JUPITER trial after its release concluded that the trial was flawed in several aspects (in fact, several articles published in the Archives of Internal Medicine refuted the claimed health benefits the very month it was released).
om all causes by 20%. Careful review of the methods and results of the JUPITER trial after its release concluded that the trial was flawed in several aspects (in fact, several articles published in the Archives of Internal Medicine refuted the claimed health benefits the very month it was released).
The main problem was that the almost 18,000 men and women in the study were only accepted as participants if they had elevated C-reactive protein (CRP) levels. CRP is an inflammatory marker that is generally found in people with inflammatory diseases. Since participants were to be disease free, this trial consisted of an unusual group of people who were supposedly “healthy,” yet had high CRP levels. The claim that a cholesterol drug could cut heart risk in healthy people is highly questionable in light of the fact that this group was not exactly representative of the average healthy person. The study was discontinued in less than two years due to the fact that there were significantly more people who had died in the untreated group (49 more than in the group that received the statin drug). Worthy to note is that 54 more people in the treated group got diabetes than in the untreated group. Although the claim was that there was a 20% relative risk decline in death from any cause among those treated with Crestor, the absolute risk for death due to any cause was 0.5%, meaning that 200 people would have to be treated with Crestor for 1.9 years (equivalent to $302,000 in profit for the drug company) to prevent one death.
 As Dr. David Brownstein pointed out in his book Drugs That Don’t Work and Natural Therapies That Do, the New England Journal of Medicine states, “absolute differences in risk are more clinically important than relative reductions in risk in deciding whether to recommend drug therapy.” Since this study was exclusively funded by Astra-Zeneca, the manufacturers of Crestor, suspicions about the tie between the findings of the researcher and the incentive of tens of billions of dollars at stake for the funders of the study seem warranted. Profit, rather than health, appears to be the driving factor behind current cholesterol recommendations.
As Dr. David Brownstein pointed out in his book Drugs That Don’t Work and Natural Therapies That Do, the New England Journal of Medicine states, “absolute differences in risk are more clinically important than relative reductions in risk in deciding whether to recommend drug therapy.” Since this study was exclusively funded by Astra-Zeneca, the manufacturers of Crestor, suspicions about the tie between the findings of the researcher and the incentive of tens of billions of dollars at stake for the funders of the study seem warranted. Profit, rather than health, appears to be the driving factor behind current cholesterol recommendations.
When you see an ad from a statin drug manufacturer with grandiose claims, you may want to look more closely at the small type. NNT (which stands for “Number Needed to Treat”) answers the question “how many people need to take a particular drug to avoid one incidence of a medical issue (such as heart attack)?” An ad for the statin drug Lipitor claimed that their drug reduced heart attacks by 36 percent based on a clinical study (industry-funded by the way). But the small type at the bottom of the ad read, “That means in a large clinical study, 3% of patients taking a sugar pill or placebo had a heart attack compared to 2% of patients taking Lipitor.” In other words, for every 100 people who took the drug over 3.3 years, three people on placebos and two people on Lipitor had heart attacks. The NNT in this case is 100. This would mean that one hundred people would have to take Lipitor for more than three years in order to prevent one heart attack. Non-industry funded clinical studies have shown an NNT as high as 250 over a five year period of time. I personally think that there are better and far safer ways to reduce the risk of a heart attack.
“Normal” Ranges – the Goalpost Keeps Moving
 For more than 30 years the normal range for total cholesterol was 150-300, which meant that only about five percent of the population had elevated total cholesterol levels. The upper limit was later changed to 240 where it remained until 1984 when it was lowered to 200. This new guideline increased the number of people at “unsafe” levels to 60% of the population. In 2004 the American Heart Association moved the goalpost even further by lowering the recommended level of LDL cholesterol from 130 to less than 100, or even less than 70 for patients at very high risk. These new guidelines instantly increased the market for statin drugs since levels this low would require the use of statin drugs to achieve. Sound scientific research and evidence to support reducing these guidelines were lacking. Moreover, eight of the nine doctors on the panel of the U.S. Government’s National Cholesterol Education Program, which created the new cholesterol guidelines, were receiving financial profit from the statin drug manufacturing companies.
For more than 30 years the normal range for total cholesterol was 150-300, which meant that only about five percent of the population had elevated total cholesterol levels. The upper limit was later changed to 240 where it remained until 1984 when it was lowered to 200. This new guideline increased the number of people at “unsafe” levels to 60% of the population. In 2004 the American Heart Association moved the goalpost even further by lowering the recommended level of LDL cholesterol from 130 to less than 100, or even less than 70 for patients at very high risk. These new guidelines instantly increased the market for statin drugs since levels this low would require the use of statin drugs to achieve. Sound scientific research and evidence to support reducing these guidelines were lacking. Moreover, eight of the nine doctors on the panel of the U.S. Government’s National Cholesterol Education Program, which created the new cholesterol guidelines, were receiving financial profit from the statin drug manufacturing companies.
Concluding Thoughts
Underlying any condition are root causes that account for imbalances which exist in the body. Excess cholesterol in the blood generally indicates that the body is producing extra amounts as a protective mechanism in response to damage in the lining of artery walls from inflammation, oxidation or other root cause. Understanding these root causes is key to both preventing and reversing heart disease. Healthy levels of cholesterol will naturally result when unhealthy factors that cause the body to produce too much in the first place are eliminated. Next month we will look at how artery walls become damaged and ways to address the underlying root causes of heart disease using natural means.
Sources:
The Cholesterol Delusion by Ernest Curtis, M.D.
The Cholesterol Myths: Exposing the Fallacy That Saturated Fat and Cholesterol Cause Heart Disease by Uffe Ravnskov, M.D., Ph.D.
Ignore the Awkward – How the Cholesterol Myths are Kept Alive by Uffe Ravnskov, M.D., Ph.D
Malignant Medical Myths by Joel M. Kauffman, Ph.D.
Drugs That Don’t Work and Natural Therapies That Do! by David Brownstein, M.D.
Know Your Fats: The Complete Primer for Understanding the Nutrition of Fats, Oils and Cholesterol by Mary G. Enig, Ph.D.
Fat and Cholesterol are Good for You! by Uffe Ravnskov, M.D., Ph.D.
Cholesterol and Your Health –Separating Fact From Fallacy by Kimberly Balas, ND, Ph.D. and Steven H. Horne, RH(AHG)
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||



