| Share |  |
 | |||
Food Allergies: Could They Be Your Problem? - Part 2
 From minor health complaints like headaches and fatigue to more serious conditions like autoimmune disease or fibromyalgia - whatever the symptom produced in the body, there is little doubt that adverse reactions that stem from food allergies are on the rise today.
From minor health complaints like headaches and fatigue to more serious conditions like autoimmune disease or fibromyalgia - whatever the symptom produced in the body, there is little doubt that adverse reactions that stem from food allergies are on the rise today.
It is believed that as many as one in four people suffer from food allergies, although the majority remain unaware that an allergic reaction to a particular food is the underlying cause of their symptoms. The latest studies and research indicates that delayed food allergies explain a variety of ailments that, otherwise, lack any clear connection.
People with these types of food allergies find little help from mainstream medicine. Other than receiving symptom-suppressing medications, they are left to live with these conditions without real solutions given to resolve them. Some doctors may even insinuate that a person’s chronic complaints are “in their head” or just caused by stress or anxiety.
What Happens in an Allergic Reaction
In order to better understand why these kinds of food allergies are on the rise and the specific factors that lead to their development, it first is important to look at what actually takes place in a food allergy reaction. The immune system is intricately involved in both immediate-onset and delayed-onset types of allergies, but there are distinct differences in the way each occur.
Immune reactions, like those created in an allergic response, involve a clash between antigens and antibodies. Antibodies are simply protein molecules the body makes to help combat disease- causing microbes. They bind to specific targets for the purpose of neutralizing their effects. 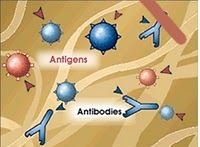 Antigens are substances that act as the “foreign invader,” stimulating the production of antibodies. They are found in the protein molecules of food, as well as in microorganisms. If a molecule even closely resembles harmful bacteria, the immune system will mount an attack against it in order to protect the body from what it perceives to be a harmful substance.
Antigens are substances that act as the “foreign invader,” stimulating the production of antibodies. They are found in the protein molecules of food, as well as in microorganisms. If a molecule even closely resembles harmful bacteria, the immune system will mount an attack against it in order to protect the body from what it perceives to be a harmful substance.
Here is what happens in a classic or immediate-onset (Immunoglobulin E or IgE for short) allergy response when a food allergen is consumed. One side of the antibody recognizes and binds to the allergic food while the other side attaches to a mast cell. A mast cell is an unstable immune cell packed with histamine and other chemical mediators that produce the allergic reaction in local tissues and organs. These cells are located in tissues throughout the body, but are especially concentrated in the gastrointestinal tract.  The immune system is now primed for action for the next time a food allergen may reappear. When that occurs, the IgE-coated mast cells clash with the food antigens, resulting in the immediate release of histamine and other allergy related chemicals that produce a range of unpleasant symptoms, such as hives, sneezing, runny nose, itchy eyes, eczema and diarrhea.
The immune system is now primed for action for the next time a food allergen may reappear. When that occurs, the IgE-coated mast cells clash with the food antigens, resulting in the immediate release of histamine and other allergy related chemicals that produce a range of unpleasant symptoms, such as hives, sneezing, runny nose, itchy eyes, eczema and diarrhea.
Delayed Food Allergy Responses
In delayed-onset food reactions, the immune system produces IgG antibodies in response to specific foods. Often the offenders are frequently eaten foods that are hard to avoid, such as milk, corn, and wheat. These antibodies form a complex with the food allergen by binding directly to the protein molecule of the food as it enters the bloodstream, rather than attaching to mast cells. The more immune complexes that are released in the bloodstream, the more the immune system reacts in defense by sending out cells called phagocytes (sometimes referred to as “pac man” cells), to “gobble” them up.
Normally these types of immune complexes are cleared from the blood by phagocytes within a few hours. However, if the offending food is continually consumed, they become too numerous for an already overtaxed immune system to handle, and it takes the body longer and longer to return to a state of balance. These immune complexes are then deposited throughout the body, producing inflammation, damaging local tissues, and setting the stage for diseases to form.
A Protective Barrier
Bear in mind that it is the larger molecules – protein fragments – of foods that precipitate the production of antibodies. A healthy gastrointestinal tract only absorbs small molecules that are products of complete digestion. In a perfect world, proteins are reduced to amino acids, carbohydrates into simple sugars and fats into fatty acids before reaching the wall of the small intestinal for absorption. These smaller molecules are not likely to provoke an allergic reaction.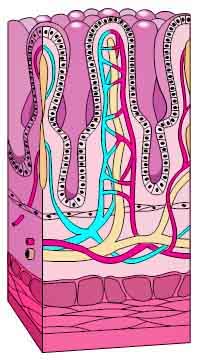 Nutrient absorption takes place through tiny “villi” (fingerlike projections) in the mucus lining of the intestinal wall. This important mucus lining, only as thick as a single cell, acts as a protective barrier to prevent toxins, microbes and large molecules of undigested foodstuffs from crossing and entering the bloodstream where they could set off an immune reaction.
Nutrient absorption takes place through tiny “villi” (fingerlike projections) in the mucus lining of the intestinal wall. This important mucus lining, only as thick as a single cell, acts as a protective barrier to prevent toxins, microbes and large molecules of undigested foodstuffs from crossing and entering the bloodstream where they could set off an immune reaction.
Leaky Gut Syndrome
If a protein is not completely digested before reaching the intestinal wall, larger molecules may seep or “leak” into the blood and lymph and provoke an allergic reaction. How does this take place? Since the cells that make up the intestinal wall are normally tightly packed together, it can only happen when spaces between these cells become enlarged from damage to this thin protective membrane.
Inflammation triggered by a food allergy reaction is one of many causes of a syndrome known as “leaky gut”. Leaky gut syndrome, termed “increased intestinal permeability” in the medical world, develops when the ability of the intestinal wall to act as a protective barrier is compromised due to such damage.
Leaky gut is a common component of both food allergies and food sensitivities. People who are allergic to foods have greater problems with intestinal permeability than non-allergic people. Little doubt exists as to the association between the two, although it remains unclear which is the greater cause or consequence. One thing is for certain – fixing either problem requires addressing both since they both are an underlying cause of many different immune system disorders and symptoms of illness.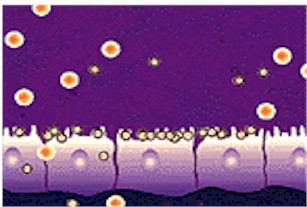 The Cascade Effect From a Leaky Gut
The Cascade Effect From a Leaky Gut
When a person has a leaky gut, antibodies may also attack the bodies own cells, which often have a similar protein structure to the large food molecules. Autoimmune diseases such as asthma, rheumatoid arthritis, lupus, chronic fatigue and fibromyalgia can result when parts of the body are attacked by this type of immune system response.
Impaired digestion and nutrient absorption is another fall-out from the inflammation and irritation produced by leaky gut syndrome and long-term food allergy reactions. Inflammation damages carrier proteins that serve to “escort” nutrients through the intestinal membrane into the bloodstream. Inadequate nutrient absorption also results from reduction in the surface area of the intestinal lining brought on by prolonged irritation and inflammation. All of these factors lead to nutrient deficiencies that contribute to everything from digestive disturbances to serious degenerative diseases.
 The brain and nervous system also are adversely affected by leaky gut. Research has shown that the likelihood of neurotoxic substances, entering the circulatory system and reaching the brain are greatly increase with increased intestinal permeability. Neurotoxic substances are clearly linked with conditions like depression, anxiety and ADD. In fact, research conducted by Dr. Michael Lyon, author of Healing the Hyperactive Brain, revealed that 75% of children with ADD have a leaky gut.
The brain and nervous system also are adversely affected by leaky gut. Research has shown that the likelihood of neurotoxic substances, entering the circulatory system and reaching the brain are greatly increase with increased intestinal permeability. Neurotoxic substances are clearly linked with conditions like depression, anxiety and ADD. In fact, research conducted by Dr. Michael Lyon, author of Healing the Hyperactive Brain, revealed that 75% of children with ADD have a leaky gut.
In addition, all of the microorganisms, toxins, and yeast more easily spread throughout the body when the structural integrity of the gut wall is compromised by leaky gut syndrome. This puts an added strain on the immune system as well as burdening the liver and its ability to detoxify the body from foreign substances.
What Causes Leaky Gut Syndrome?
Without a doubt, leaky gut is a primary causal factor in food allergies. But what factors are involved in its development? Bear in mind that some of these same factors also play a significant role in the development of food allergies, as the two are so intertwined.
Anything that irritates or produces damage to the gut wall such as:
- Food allergens – continuing to eat a food allergen (especially gluten) causes damage to the lining of the gut over time – eating excessive amounts of a particular food, especially one that is high in allergy forming proteins such as cow’s milk
 (clearly increases gut permeability according to the Journal of Gastroenterology), wheat, eggs, certain nuts and other common food allergens
(clearly increases gut permeability according to the Journal of Gastroenterology), wheat, eggs, certain nuts and other common food allergens - Drugs – especially NSAIDS (non-steroidal anti-inflammatory drugs such as aspirin and ibuprofen) – blocks the prostaglandin pathways that enable the body to repair itself – tears down the lining of the stomach and intestines - long term use of corticosteroid drugs depresses immune system function, and encourages fungal growth
- Lectins – found in many whole grains and legumes – damages cells in intestinal lining and creates imbalance in gut bacteria
- Viral, bacterial, parasitical or yeast infection – produces inflammation in the gut that is a result of the immune system’s attack on the “invader”
- Extreme stress or trauma (surgery, injuries, high fever, infections, overly rigorous-exercise) - stress robs the body of glutamine, the primary fuel for the intestinal lining – creates inflammation - slows down digestion – affects immune system’s ability to produce sufficient antibodies
- Alcohol, caffeine, chemicals and additives in processed foods – irritates the gut wall and decreases the number of friendly bacteria needed for a healthy gut
- Candida – fungal organism that forms root-like structures that penetrate and damage the intestinal lining as it searches for food – overgrowth disrupts balance of intestinal bacteria – inhibits intestinal mucus lining from functioning properly

Absence of good bacteria to maintain intestinal health – good bacteria provides fuel for intestinal cells and deprives disease-causing bacteria of nutrients. The presence of good bacteria is diminished by:
- Overuse of antibiotics – disrupts balance of bacteria – can cause Candida overgrowth – reduces B vitamin production – increases homocysteine levels
- Antacid use – neutralizes hydrochloric acid needed to break down proteins, destroys harmful microorganisms and enables mineral absorption necessary for digestive enzyme production
- Birth control pills – disrupts balance of bacteria
- High refined carbohydrates and sugar diet – sugar throws off balance of bacteria – responsible for high blood sugar associated with inflammation – impairs good digestion by creating acidity and depleting minerals needed for digestive enzymes to work properly
- Chlorinated (tap) water – destroys good bacteria
- Chemotherapy – creates inflammation in small intestine – hinders absorption of nutrients
Enzyme and nutritional deficiencies – it is large molecules of undigested food that enlarge spaces between cells in intestinal lining - foods cannot be digested well or assimilated effectively apart from sufficient amounts of the right enzymes and nutrients.
 Poor liver function – the liver is the major detoxification system that processes everything that enters the mouth – processing too many chemicals, drugs, food allergens, etc., produces large amounts of inflammatory toxins excreted into intestines via bile
Poor liver function – the liver is the major detoxification system that processes everything that enters the mouth – processing too many chemicals, drugs, food allergens, etc., produces large amounts of inflammatory toxins excreted into intestines via bile
Processed & GMO foods – lacking in nutrients, low in fiber needed to absorb toxins and move wastes out of the body – full of chemical additives, preservatives and flavorings – altered foods difficult for body to break down – digestive stress produces inflammation
Early introduction of solid foods to infants – intestinal lining of a child less than a year is not mature enough to keep potential allergens from entering the bloodstream.
To prevent antibodies to potentially allergic foods from building up and causing food allergies later in life:
- Breastfeed only for the first six months – breastmilk is rich in a substance that coats the lining of the intestines and helps prevent potential allergens from entering blood stream.
- Start on solid foods that are lower in protein such as vegetables, fruits and rice until the child is a year old.
- Restrict all forms of wheat, soy or dairy for at least one year.
- Wait as late as 18 months to introduce highly allergic foods such as tomatoes, shellfish, egg whites and peanut butter.
- Have children eat a wide variety of foods so they will not increase their risk of becoming allergic to a food by overeating one particular kind (such as too much bread, pizza, crackers, cookies etc., all of which contain wheat flour).
 With the many factors that can contribute to leaky gut syndrome and food allergies, it is safe to say that nearly everyone has experienced one or more of them in their lifetime. The good news is that our liver acts as a back-up for digestion and detoxification in the event toxins or undigested foodstuffs do slip through a marginally leaky gut.
With the many factors that can contribute to leaky gut syndrome and food allergies, it is safe to say that nearly everyone has experienced one or more of them in their lifetime. The good news is that our liver acts as a back-up for digestion and detoxification in the event toxins or undigested foodstuffs do slip through a marginally leaky gut.
Therefore, as long as the immune system, digestive processes, and detoxification processes of the liver are working well, the lining of small intestine can usually repair and replace itself in a matter of days. But if any of these factors are chronic or ongoing, or if the detoxification processes of the liver are overtaxed from excessive amounts of toxins and chemicals, it is difficult for the gut to heal.
Do You Have Leaky Gut Syndrome?
How do you know if you may have leaky gut syndrome? You can get a pretty good idea by rating yourself on whether or not you experience any of the following symptoms. Select the appropriate number that best represents what extent you experience any of the symptoms or conditions listed in the “quiz” below.
Leaky Gut Questionnaire
0 – Not applicable
1 – Rarely present – very mild
2 – Often – moderate
3 – Almost always – severe
_____ Constipation and/or diarrhea
_____ Abdominal pain or bloating
_____ Mucus or blood in stool
_____ Joint pain or swelling
_____ Chronic or frequent fatigue
_____ Food allergies, sensitivities or intolerance
_____ Sinus or nasal congestion
_____ Chronic or frequent inflammation
_____ Eczema, skin rashes or hives
_____ Asthma, hay fever or airborne allergies
_____ Confusion, poor memory or mood swings
_____ Use of NSAIDS (aspirin, ibuprofen, etc.)
_____ History of antibiotic use
_____ Alcohol consumption
_____ Ulcerative colitis, Crohn’s or Celiac
Total Score: ______
If you scored:
0-5 – Leaky Gut less apt to be present
6-10 – Leaky Gut may possibly be present
11-19 – Leaky Gut probably present
20 + - Leaky Gut most certainly present
Conclusion:
The intestinal wall acts as a gateway to absorb needed nutrients into our bloodstream in order to feed vital cells, tissues and organs. Equally significant is its role in keeping harmful toxins, bacteria and incompletely digested food from entering the bloodstream. If holes develop in that wall, it poses a threat as serious as gaps in the defensive front line of an army. The "enemy" can slip right past and cause destruction.
Since 60% of the immune system resides in the gut, one sure way to strengthen it and our health is to close the gaps of a leaky gut. By doing so, you will greatly reduce the likelihood of a food allergy reaction in addition to preventing the development of numerous health problems.
Next month we will look at ways to heal a leaky gut and reduce the occurrences of food allergies in the process. You will also learn how to identify what foods you may be allergic to and how to do an elimination diet that will end the effects of food allergies and allow your body to heal.
Sources:
- Food Allergy and Food Intolerance: The Complete Guide to their Identification and Treatment by Jonathan Brostoff, M.D. and Linda Gamlin
- The Food Allergy Cure by Ellen Cutler, M.D.
- Going Against the Grain by Melissa Diane Smith
- http://www.drbralyallergyrelief.com/igg.html
- http://www.naturalnews.com/022556_food_allergies_disease.html
- http://www.excelonhealth.com/ExConditions_FoodAllergy.html#N1
- http://www.consumerhealth.org/articles/display.cfm?ID=20010214042825
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||



