| Share |  |
 | |||
Better Bone Health - Solutions for Osteoporosis
 A growing health concern for women today is preventing or, in some cases, reversing a condition affecting the bones that has dramatically increased over the last thirty years. Over 10 million Americans have been diagnosed with osteoporosis and another 34 million with osteopenia (a milder form of decreased bone density). Although these conditions also affect men, approximately 80% of all cases are women. In fact, it is believed that 30% of women over the age of 50 have either osteoporosis or osteopenia.
A growing health concern for women today is preventing or, in some cases, reversing a condition affecting the bones that has dramatically increased over the last thirty years. Over 10 million Americans have been diagnosed with osteoporosis and another 34 million with osteopenia (a milder form of decreased bone density). Although these conditions also affect men, approximately 80% of all cases are women. In fact, it is believed that 30% of women over the age of 50 have either osteoporosis or osteopenia.
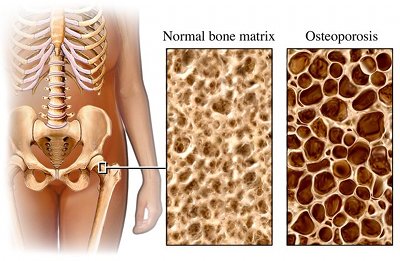
Osteoporosis, which literally means “porous bones,” is a degenerative condition characterized by bones that progressively deteriorate in strength and mass. Bones that continue to weaken become more fragile and susceptible to fractures, especially of the hip, spine and wrist. Not only can spinal fractures and collapsing vertebrae lead to chronic pain and loss of height, but they also can cause the disfiguring forward-stooped posture known as “dowager’s hump” that reduces the heart and lung capacity of the individual. Moreover, a large percentage of the elderly who experience hip fractures end up in nursing homes and die within a year from fracture-related complications.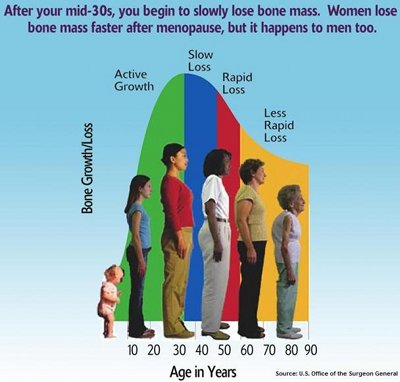
Needless to say, it is important to take care of the health of our bones. Not only do bones provide a framework of support for our body and protect the softer tissues underneath, they also serve as a storage site for essential minerals and a manufacturing plant for blood cells - both red blood cells that carry oxygen to the rest of the body and white blood cells that play a key role in the immune system. In addition, they help manage the acid-alkaline balance of the blood that is so crucial to maintain for good health, often to the point of sacrificing their own nutrients and resources.
Understanding the Bone-Building Process
Even though bones are regarded as static “set in stone” parts of our body, they are actually composed of living cells and tissues that undergo continuous modification throughout life in a process called “remodeling.” Old and damaged bone is constantly being removed and new bone tissue is produced to take its place.
stone” parts of our body, they are actually composed of living cells and tissues that undergo continuous modification throughout life in a process called “remodeling.” Old and damaged bone is constantly being removed and new bone tissue is produced to take its place.
The remodeling process that determines if bones are weakened or healthy is governed by the interaction of two types of cells. Cells known as osteoclasts work to remove old and injured bone tissue by dissolving the mineral matrix they contain. They then lay down a protein mix that helps stimulate other cells known as osteoblasts. Osteoblasts form mineralized bone by producing a collagen-based substance and then drawing calcium and other minerals into the bone to combine with it.
If either of these types of cells is overactive or fails to function optimally, one of two things will occur: too much bone may be broken down or not enough good quality bone will be laid. Optimizing the function of both types of cells ensures that old damaged weak bones will be removed (a process known as resorption) and new strong bone will be deposited (remodeling). Osteoporosis occurs when an imbalance exists between these two types of cells and bone tissue is broken down and removed faster than it can be replaced.
Are Drugs the Solution?
Osteoporosis drugs are usually recommended for people who show a decline in bone mineral density. Bisphosphonates is the class of drugs commonly used today by conventional medicine in osteoporosis treatment. Fosamox, Boniva, Actonel, Reclast, Aredia and Zometa are names of the more common of these particular drugs. The purpose of these drugs is to increase bone mineral density. 
When bisphosphonates are taken, compounds in them attach to bone tissue and are then absorbed by the osteoclasts. Once absorbed, they poison a certain enzyme in a key pathway and the osteoclasts die. The problem with this is that both types of cells need to function normally for bones to be healthy. Poisoning the osteoclasts is like taking one half of the rebuilding process (resorption) out of the picture. This means that if the bone is ever injured, the normal healing process cannot take place. Rebuilding bone in this manner is like repairing a road with potholes by just filling in the potholes with pavement material instead of taking up the damaged road and laying down new pavement. Obviously, the latter would create a much stronger road. Even though bones initially appear denser, they are actually weak and of poor quality because of the fact that old damaged bone is not removed.
Granted, BMD scans typically show marked improvement over the first year of a person taking these drugs because bone loss is halted and bones continue to build. However, continued use of the drug eventually stops the process of bone formation as well. The consequences of long-term use is actually less protection against debilitating fractures due to the fact that the natural ability of the body to repair and rebuild is blocked from the interference of the drug’s action on its normal processes.
Another problem with these drugs is that once the drug binds to the bone and poisons the osteoclasts, the body has no mechanism to rid itself of the bisphosphonate. Since there is such a prolonged half-life with most of these drugs (even in excess of 10 years), the long-term adverse effects may not be reversible (a drug’s “half-life” indicates the amount of time it takes for 50% of the drug to be eliminated from the body). These drugs are also linked with a number of side effects including severe musculoskeletal pain, ulcers of the esophagus, upper GI irritation, and, in rarer cases, a serious bone-related jaw disease called osteonecrosis, commonly referred to as “dead jaw.” The latter is a debilitating condition that often does not respond to surgical or medical treatments. Reports of atypical femur fractures and esophageal cancer in people taking these drugs for a period of years are on the rise as the number of people taking these drugs in excess of five years increases.
Keep in mind when you hear or read advertisements cla iming a high percentage of reduced risk of fracture rates from taking a certain bisphosphonate drug that the percentage is based on “relative risk reduction” versus “absolute risk reduction,” which is an extremely misleading manipulation of numbers that does not take into account the NNT (number needed to treat) factor. The NNT factor is the most significant factor to weigh when determining whether or not a drug should be used for treatment. As an example, a study on fracture rates of thousands of high-risk postmenopausal women would have one half of the women taking the drug and the other half taking a placebo. If 2% of the placebo group experienced fractures versus 1% of those who took the drug, the absolute risk reduction with the drug use would be 1%, which translates to one woman out of a thousand receiving benefit from the drug. Considering the risks and side effects of these drugs, this percentage is not that significant. However, when the manufacturer uses the relative risk reduction method, they will advertise that the drug reduced the risk of fractures by 50% since 1% is half of 2%.
iming a high percentage of reduced risk of fracture rates from taking a certain bisphosphonate drug that the percentage is based on “relative risk reduction” versus “absolute risk reduction,” which is an extremely misleading manipulation of numbers that does not take into account the NNT (number needed to treat) factor. The NNT factor is the most significant factor to weigh when determining whether or not a drug should be used for treatment. As an example, a study on fracture rates of thousands of high-risk postmenopausal women would have one half of the women taking the drug and the other half taking a placebo. If 2% of the placebo group experienced fractures versus 1% of those who took the drug, the absolute risk reduction with the drug use would be 1%, which translates to one woman out of a thousand receiving benefit from the drug. Considering the risks and side effects of these drugs, this percentage is not that significant. However, when the manufacturer uses the relative risk reduction method, they will advertise that the drug reduced the risk of fractures by 50% since 1% is half of 2%.
How Relevant is Bone Mineral Density Testing?
Bone Mineral Density (BMD) testing determines the amount of mineralized tissue in the bones and is widely regarded by health organizations, drug companies, doctors and the medical community as the primary means for diagnosing osteopenia or osteoporosis. According to the World Health Organization, osteoporosis is defined as a BMD score below -2.5 standard deviations of normal. Osteopenia is defined as BMD from -1.0-2.5 standard deviations below n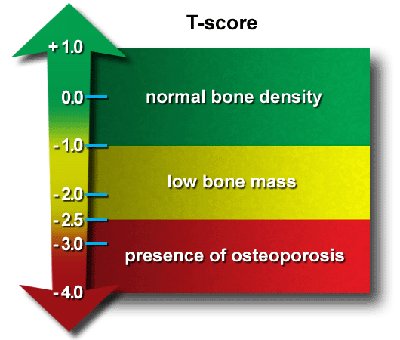 ormal.
ormal.
People do not often realize that the levels considered normal (referred to as T-score) are based on the bone density of average women during young adulthood (approximately age 20-29). Bear in mind that bones reach their maximum levels of density and strength at these ages. According to BMD standards, natural age-related decrease in bone density is automatically categorized as abnormal even though the great majority of individuals will never fracture a bone due to age-related decline in bone mass. Following these standards would mean that two-thirds of older women in western countries would be in need of treatment for osteoporosis.
The use of BMD testing alone to determine the health of bones can be misleading when you take into account the following:
- BMD testing only regards the quantity of bone and its degree of thickness and does not reflect the overall health or strength of the bones. In other words, it is possible to have strong thin bones as well as weak thick bones.
- Low bone mineral density does not equate with osteoporosis as it is only one factor in its development.
- Age-related decline in bone mass does not necessarily result in fracture of bones.
- Fracture rates cannot be predicted by a BMD scan in spite of the fact that the World Health Organization claims each standard deviation decrease in BMD doubles the risk of fracture.
 The truth of the matter is that loss of bone mass with age is actually quite normal. The process of bone remodeling is generally balanced until the fourth decade of life when resorption becomes slightly greater than bone formation. The greatest bone loss occurs in the years immediately after menopause when estrogen levels decline which is why women lose bone approximately four times more rapidly than men. After age 65, the loss of bone mass slows down.
The truth of the matter is that loss of bone mass with age is actually quite normal. The process of bone remodeling is generally balanced until the fourth decade of life when resorption becomes slightly greater than bone formation. The greatest bone loss occurs in the years immediately after menopause when estrogen levels decline which is why women lose bone approximately four times more rapidly than men. After age 65, the loss of bone mass slows down.
Rather than address what is causing the disease process that underlies bone loss, the focus of most physicians is solely on improving bone density. The fact is that bone loss is not just a weakening of bones but is rather indicative of deficiencies and imbalances that affect the overall physiology of the body. Bones need to be healthier – not just thicker. Both the quantity and quality of bones should be taken into account when evaluating bone health.
Are you at Risk for Osteoporosis?
Even though increasing bone mineral density has not conclusively been shown to reduce the risk of bone fractures, a lower BMD is one valid marker indicating a risk for developing osteoporosis. Multiple factors exist that either affect the normal function of osteoclasts and osteoblasts or in some other way cause bones to weaken and become osteoporotic. Factors considered “unchangeable” that may increase your risk of developing osteoporosis are:
- Genes – genes control the size and shape of bones. Genetic mutations can cause dysfunctions of osteoclasts and osteoblasts that can result in weakened bones.
- Gender – women typically are four times more likely than men to have osteoporosis. Women have lighter, thinner bones and lose bone faster than men due to the effects of estrogen loss associated with menopause. Longer life spans add to the likelihood that they will develop osteoporosis.
- Age – bones become thinner and weaker with age
- Race/Ethnicity – people who are white or of Asian descent are at the greatest risk of osteoporosis
- Frame Size – people with thin, small body frames tend to have a higher risk because they typically have less bone mass to draw from as they age
- Family History – people whose parents have a history of fractures may be at greater risk. A maternal history of hip fracture is particularly significant.
- Medical conditions – weight-loss surgery, Crohn’s disease, celiac disease, Cushing’s disease, hyperparathyroidism, Paget’s disease and rheumatoid arthritis either affect bone health or are the result of abnormal function of osteoblasts or osteoclasts.
Considering the Controllable Causes and Solutions
 Osteoporosis is a complex condition that encompasses a wide range of dietary, lifestyle, hormonal, and environmental factors. While the risk factors cited above may be valid indicators that a person could develop osteoporosis, the reasons that bone health actually weakens generally involve a number of other factors involving overall health that are indeed controllable. For any chronic degenerative condition in the body, the real solution is to examine where and how the body is out of balance and address the underlying root causes.
Osteoporosis is a complex condition that encompasses a wide range of dietary, lifestyle, hormonal, and environmental factors. While the risk factors cited above may be valid indicators that a person could develop osteoporosis, the reasons that bone health actually weakens generally involve a number of other factors involving overall health that are indeed controllable. For any chronic degenerative condition in the body, the real solution is to examine where and how the body is out of balance and address the underlying root causes.
There are many natural ways to support bone health that do not involve the use of drugs to keep them strong and prevent fractures. In the concluding part of this article next month, I will address the real factors that contribute to osteoporosis and, more importantly, give definitive natural solutions for a whole-body approach to building healthier bones.
Sources:
The Whole-Body Approach to Osteoporosis by R. Keith McCormick, DC
The Myth of Osteoporosis by Gillian Sanson
Drugs that Don’t Work and Natural Therapies That Do by David Brownstein, M.D.
http://www.betterbones.com/osteoporosis/top10myths.aspx
http://www.betterbones.com/osteoporosis/risks-benefits.aspx
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||


