| Share |  |
 | |||
Using Thermography to Detect Breast Cancer Earlier
 Prevention and early detection of breast cancer should be a top health priority for women today. During the past half century, incidents of breast cancer have tripled in the United States. Current estimates indicate that one in eight women will develop breast cancer during their lifetime, making this type of cancer three times more common than other gynecological cancers.
Prevention and early detection of breast cancer should be a top health priority for women today. During the past half century, incidents of breast cancer have tripled in the United States. Current estimates indicate that one in eight women will develop breast cancer during their lifetime, making this type of cancer three times more common than other gynecological cancers.
Out of the more than 230,000 new cases of invasive breast cancer diagnosed in the US, at least 40,000 women will lose their lives to this dreaded disease. And a report issued by the National Cancer Institute in April of 2015 predicts an estimated 50 percent increase in breast cancer diagnoses rates by the year 2030.
The life-saving benefit of detecting breast cancers at the earliest possible stage is without dispute among all experts and health associations. However, differences do exist with regards to what is the safest and most effective type of screening and how early and often women should be tested.
All of the standard means of “early” detection of a breast cancer tumor - breast self-exams, gynecological examinations, mammogram screenings, ultrasounds, MRIs, etc. – 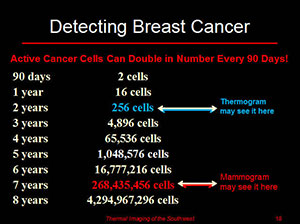 rely on observing the anatomy of an existing tumor. The problem is that breast cancer tumors typically take as many as six to eight years to grow to a size detectable with these means.
rely on observing the anatomy of an existing tumor. The problem is that breast cancer tumors typically take as many as six to eight years to grow to a size detectable with these means.
Breast Thermography – an Alternative Screening Option
Breast thermography is an additional option women should consider to protect their health against the ravages of breast cancer. While lesser known and promoted, medical breast thermography (also known as DITI - Digital Infrared Thermal Imaging) is a safe and highly sensitive as well as scientifically proven clinical screening test for detecting changes that can indicate early stage breast disease years before what would be possible with other means of detection.
Although infrared technology has been used since the 1970's, the use of thermography as an adjunctive breast cancer risk assessment screening tool was first approved by the FDA in 1982. More than 800 peer-reviewed studies on the use of breast thermography have been published in medical literature and a research bank of well over 300,000 women tested with infrared breast imaging and followed for longer than twelve years now exists. The American Journal of Radiology published a study in January 2003 that 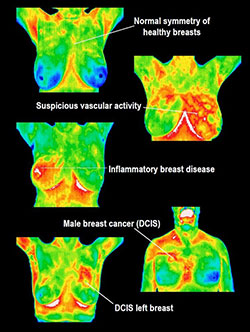 confirmed breast thermography as a safe noninvasive procedure that can help to prevent unnecessary breast biopsies.
confirmed breast thermography as a safe noninvasive procedure that can help to prevent unnecessary breast biopsies.
At an “International Symposium on Detection and Prevention of Cancer” held in 1976, medical thermography was established by consensus as the highest risk marker for the possibility of the presence of an undetected breast cancer. Moreover, an abnormal thermogram is considered eight times more significant as a future risk indicator for breast cancer than a first order family history. Repeated abnormal thermograms are associated with a 22 times higher risk of future breast cancer.
Breast thermography differs from mammography in that it is a non-invasive evaluation of the physiology of breast tissue and visually captures the presence of inflammation in breast tissue that often accompanies precancerous changes in the breast. It is not intended to be a stand-alone method for diagnosing breast cancer nor is it meant to replace mammography or other diagnostic tests that measure anatomical abnormalities in breast tissue.
According to the International Academy of Clinical Thermology (IACT), studies show that adding breast thermography to a woman’s regular health check-ups increases survival rates from breast cancer by approximately 61 percent. In places like Europe and Canada, thermography is considered mainstream for routine screenings of healthy breasts while mammograms are used as a second line of screening for diagnostic purposes.
How Does Breast Thermography Work?
Thermography uses ultra-sensitive infrared digital cameras to capture infrared radiation emitted from the surface of the skin. Metabolic activity within the breast produces heat that is carried to the skin surface by the blood supply. Sophisticated computer software analyzes and translates this information into  high-resolution digital images that use a spectrum of colors to indicate any increase or decrease in the amount of infrared radiation emitted from the surface of the body.
high-resolution digital images that use a spectrum of colors to indicate any increase or decrease in the amount of infrared radiation emitted from the surface of the body.
When visualized with thermography, normal breast tissue produces a characteristic temperature pattern. Fast-growing, abnormal breast tissue (whether pre-cancerous or cancerous) produces greater heat due to its faster metabolism.
The formation of new blood vessels is the other primary cause of temperature changes in the breast. As breast cells begin to multiply abnormally, additional blood vessels must be created to supply them with the extra nutrients their accelerated growth demands. Unlike normal blood vessels, blood vessels created to support cancer cells grow in characteristically abnormal patterns that generate more heat than the tissues that surround them. Thermography is the only technology that can detect the formation of new blood vessels that occur when a tumor reaches the size of a pinhead (approximately two years into its growth).
During a thermogram, the heat sensing infrared camera captures the changing heat and vascular patterns of breast tissue that take place in the initial and subsequent phases of a cancerous growth. The different colors seen on a thermogram report reflect various types of changes in the breasts and surrounding regions of the body as well. “Hot spots” are shown in red and indicate areas of high 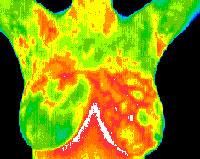 inflammation that denotes some type of abnormality or potential for cancerous growth.
inflammation that denotes some type of abnormality or potential for cancerous growth.
Breast thermograms show a highly specific thermal pattern for each individual woman that remains constant over the years unless an underlying condition causes a change. An abnormal thermogram does not automatically mean that a woman has breast cancer. Other conditions can cause “hot spots” including benign tumors, fibrocystic breast disease, mastitis and other non-cancerous conditions. Once a woman obtains a baseline thermogram, repeated screenings can help to differentiate between a cancerous tumor and other benign disorders that will cool down as they resolve. If an area of tissue is indeed cancerous, it will remain “hot” or become even hotter.
 Pros and Cons of Breast Thermography and Mammography
Pros and Cons of Breast Thermography and Mammography
It is important to understand that neither thermography nor mammography diagnose cancer as that process can only take place under a microscope. Mammography only diagnoses physical or structural abnormalities and thermography only evaluates biochemical and blood vessel activity. The purpose of this article is to help you learn how both of these imaging technologies can play a vital role in protecting your breast health and what the limitations and drawbacks are of each.
TIMING OF DETECTION
Since a thermography screening can “see” changes at the cellular level along with abnormal physiological processes related to inflammation and/or increased tumor related blood flow, it offers a far earlier opportunity for detecting breast disease than what is possible through self-examination, doctor examination, or mammography alone. Studies suggest that a breast thermogram can detect pre-cancerous activity and early tumor formation as much as eight years before any other type of test.
Discovering a potentially cancerous growth years before it reaches a size detectable with conventional means affords a woman a greater window of time to address and reverse the underlying causes with healthy diet and lifestyle modifications while  opportunity still exists. Subsequent thermograms may safely be performed as often as desired to provide invaluable feedback on how nutritional and lifestyle methods are working (or not) to reverse the disease process.
opportunity still exists. Subsequent thermograms may safely be performed as often as desired to provide invaluable feedback on how nutritional and lifestyle methods are working (or not) to reverse the disease process.
If the thermogram is still abnormal with no observed improvement, then a woman can get a breast ultrasound. If the ultrasound is suspicious, then a mammogram would be in order to pinpoint the exact location of the existing tumor for a biopsy. The earlier a biopsy is done if it is indeed cancer, the greater the chance for a full recovery without having to have a mastectomy or go through invasive and potentially harmful treatments such as chemotherapy and radiation.
ACCURACY OF DETECTION
False Negatives
While mammograms are beneficial the majority of the time in detecting a breast cancer up to two years before detection would be possible with a physical examination, approximately one out of five mammograms turn out to be “false negatives”. A false negative is a screening result that appears normal even though cancer is present. Not only do these types of results give women a false sense of security but they can also dangerously delay a cancer diagnosis.
 The primary factor that contributes to “false negatives” with mammography is dense breast tissue that is often found among pre-menopausal women younger than 50. About a third of all breast cancers occur in this category of women.
The primary factor that contributes to “false negatives” with mammography is dense breast tissue that is often found among pre-menopausal women younger than 50. About a third of all breast cancers occur in this category of women.
About half of the time, accurate detection of a breast cancer tumor with mammograms can also be difficult in women with breast implants, depending on the type and placement. Cancers that originate below the armpits can be missed with mammograms as well since they only examine the breast tissue compressed between the two plates.
Breast thermography may be a better screening choice for younger women since a potential tumor cannot as easily escape detection in dense breast tissue as it can with palpation, mammograms and other imaging tests. Besides women with dense breast tissue, breast thermography is particularly beneficial for women who are pregnant or nursing in addition to those with breast implants, fibrocystic disease, a history of biopsies or who take hormone replacement therapy as mammograms are either less sensitive or safe for women in these categories.
False Positives
A false positive result refers to cases in which abnormal spots identified as “suspicious” for cancer with a mammogram turn out to be benign. Besides the psychological and emotional distress involved, a false positive result usually means more tests and follow-up visits, more radiation exposure, and oft times unnecessary invasive procedures including fine-needle aspiration, biopsies and sometimes even unnecessary surgery. The more mammograms a woman has, the greater the chance of a false positive result.
A study that analyzed data from more than 386,000 mammograms from 170,000 women over a ten year period estimated that 61 percent of women screened annually and 42 percent screened biannually were called back at least once for a follow-up test that showed they in fact did not have cancer. Women who  were screened annually also had a greater probability of having an unnecessary biopsy over the ten year period (seven to nine percent of women) compared with five to six percent of those who were screened less frequently.
were screened annually also had a greater probability of having an unnecessary biopsy over the ten year period (seven to nine percent of women) compared with five to six percent of those who were screened less frequently.
Breast thermography can be used in conjunction with mammograms to help eliminate the need for many unnecessary biopsies and the high cost and emotional suffering that accompanies them.
It is difficult to access “false positive” rates with breast thermography since a suspicious result only points to inflammation and chemical and vascular changes in the breast tissue that could mean the possible development of a cancerous tumor. Since not all changes in the surface of the skin’s temperature are caused by cancer, what is picked up by a breast thermography may be some harmless breast condition. Moreover, when a thermography test shows a suspicious area that cannot be confirmed soon after as a cancer with diagnostic tests, it may still turn out to be cancer years later. In other words, the thermography result is not necessarily inaccurate just because a cancer is not yet developed to a size detectable by other means of technology.
Overdiagnosis and Treatment
Overdiagnoses and overtreatment is a further consequence of the all too frequent occurrences of false positives from annual mammogram screenings. The fact is that approximately 80 percent of lumps found in the breast are not cancerous but rather fibrosis, cysts or benign tumors.
A 2011 meta-analysis by the Cochrane Database of Systemic Reviews revealed that mammography breast cancer screening led to 30 percent rate of overdiagnosis and overtreatment, which actually increased the absolute risk of developing cancer by 0.5 percent. Researchers determined that for every 2,000 women screened throughout a 10 year period, one will have her life prolonged due to the screening while 10 healthy women who would not have been diagnosed apart from the screening will be treated unnecessarily.
Impact on Mortality
I n a new study recently published in JAMA Internal Medicine (July, 2015), researchers reported no significant correlation between the number of screening mammograms performed on 16 million women from 547 U.S. counties and fewer breast cancer deaths. The number of breast cancer diagnoses indeed rose with the number of screenings but the amount of breast cancer deaths over the next 10 years remained the same. The conclusion suggested by the researchers was that breast cancer screening may lead to overdiagnosis more than fewer deaths.
n a new study recently published in JAMA Internal Medicine (July, 2015), researchers reported no significant correlation between the number of screening mammograms performed on 16 million women from 547 U.S. counties and fewer breast cancer deaths. The number of breast cancer diagnoses indeed rose with the number of screenings but the amount of breast cancer deaths over the next 10 years remained the same. The conclusion suggested by the researchers was that breast cancer screening may lead to overdiagnosis more than fewer deaths.
POTENTIAL DANGERS
Compression
Should a cancerous growth exist, the compression of breast tissue that must of necessity take place during a mammogram session is not only painful but it can potentially lead to a dangerous spread of the cancerous cells due to the rupturing of blood vessels in and around the tumor. The pressure that the mammogram machine puts on each breast during the compression process is equivalent to a 50-pound weight.
Breast thermography imaging is completely safe, non-invasive and painless. It is as easy as getting your picture taken because that is all it basically involves.
Radiation Exposure
The good news is that digital mammography (also known as Full-Field Digital Mammography or FFDM) has replaced former x-ray films and is currently available in most parts of the country. Besides the advantages of higher quality images that can be manipulated for better views and greater accuracy, the newer technology delivers a lower radiation dose than previous standard mammograms.
Another even newer technology is 3-D breast imaging (also known as breast tomosynthesis), a mammography system in which an x-ray tube moves in an arc over the breast during the exposure, taking multiple x-rays along the way that are then computed together into a 3-D image. This imaging technology is  typically used with women with dense breast or areas of suspicion. While 3-D imaging allows for improved detection of cancer and fewer patients recalled for additional imaging, the huge disadvantage is that it exposes a woman to even higher doses of radiation than a standard mammogram. If that were not a great enough concern, women are still expected to undergo the traditional 2-D mammogram at the same time, further multiplying radiation exposure. According to Fran Visco, president of the National Breast Cancer Coalition, there is not data to prove that 3-D tomosynthesis finds more cancer or saves lives. Her view is that this new technology should not be used outside of a clinical trial.
typically used with women with dense breast or areas of suspicion. While 3-D imaging allows for improved detection of cancer and fewer patients recalled for additional imaging, the huge disadvantage is that it exposes a woman to even higher doses of radiation than a standard mammogram. If that were not a great enough concern, women are still expected to undergo the traditional 2-D mammogram at the same time, further multiplying radiation exposure. According to Fran Visco, president of the National Breast Cancer Coalition, there is not data to prove that 3-D tomosynthesis finds more cancer or saves lives. Her view is that this new technology should not be used outside of a clinical trial.
Even though digital mammography reduces radiation amounts in comparison to previous film x-rays, the fact remains that ionizing radiation is a known contributor to cancer and radiation exposure from all sources adds up over the years. Consequently, imaging tests that use radiation should be used on a limited basis as possible especially when it comes to the breasts of pre-menopausal women that are highly sensitive to radiation induced DNA damage. No evidence exists that the benefits of mammograms in women younger than 50 outweighs the risks of radiation exposure. The degree of susceptibility to radiation induced DNA damage is also associated with women who carry mutated "breast cancer genes" including BRCA1, BRCA2, as well as the genes ATM, CHEK2 and A-T. Since these women are less able to repair damage to DNA, radiation exposure is more dangerous for them.
Frequency of Screening
Even with potential dangers from radiation exposure, the American Cancer Society still recommends that women get annual mammograms starting at age 40 in spite of the fact that recommendations were revised in November of 2009 by a federal advisory board (the US Preventive Services Task Force). The newer guidelines for average-risk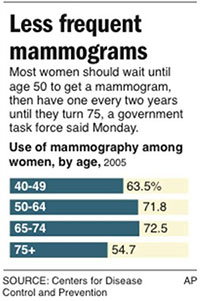 women state that annual mammograms are not necessary for women under age 50 and that screenings were recommended only every two years and then just for women between the ages of 50 and 74. The Task Force concluded that the risk of additional and unnecessary testing far outweighed the benefits of annual mammograms.
women state that annual mammograms are not necessary for women under age 50 and that screenings were recommended only every two years and then just for women between the ages of 50 and 74. The Task Force concluded that the risk of additional and unnecessary testing far outweighed the benefits of annual mammograms.
Studies show that women who follow the American Cancer Society guidelines receive NO additional protection against aggressive breast cancer, but actually experience greater harm through increased false positives and unnecessary treatments when compared with woman who start mammogram screening after age 50 and have them done every other year. One 2010 study showed induced incidences of cancer and increased rate of fatal breast cancers at the rate of 20-25 cases per 100,000 on women aged 40-80 who received annual mammogram screenings.
Women who elect to use breast thermography for routine screenings should get an initial thermogram that provides a base line of their unique thermal pattern. A subsequent session, about three months later, is recommended to assure that thermal patterns remained unchanged. 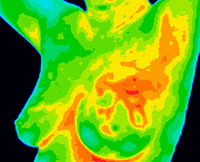 An annual thermogram evaluation is recommended in women over the age of 40 to detect any changes that may occur. For higher risk women and maximized early detection, the recommendation to start annual screenings is age 30.
An annual thermogram evaluation is recommended in women over the age of 40 to detect any changes that may occur. For higher risk women and maximized early detection, the recommendation to start annual screenings is age 30.
Although a woman can begin thermography screenings at any age, the ideal age range for an initial thermogram is 25 as this provides an early benchmark to optimize the accuracy of thermograms taken in later years. Subsequent thermograms for younger women need only be done every few years until they begin annual screenings at the appropriate age (30 or 40 depending on risk factors and/or personal choice).
Concluding Thoughts
No type of breast cancer screening truly prevents breast cancer. But a thermal imaging test capable of capturing the initial phases of the disease process is invaluable in protecting a woman from becoming a breast cancer statistic. The fact that the procedure is non-invasive, pain free and absent of any possible harmful effects is a huge plus. The best part about thermography is that it gives a woman the gift of a larger window of time - time to take the necessary steps to reverse the disease process and practice preventative care while it is still possible.
Mammograms do play a vital role in helping to identify existing cancerous growths and pinpoint their exact location when needed. Unfortunately, they are not without harmful effects and may not be the best option for annual screenings for healthy women, especially premenopausal women and/or those under the age of 50.
Every woman should take their health in their own hands and do their part to protect their breast health by performing regular self-examination, getting routine medical check-ups and by making educated choices with regards to the type and frequency of breast cancer screening imaging options.
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||



