| Share |  |
 | |||
Food Allergies - Could Gluten Be Your Problem?
 An intolerance to wheat and/or gluten ranks high on the list of the most common causes of allergic reactions to food. This is not surprising when you take into account how extensively foods derived from this grain of choice are consumed in the typical American diet.
An intolerance to wheat and/or gluten ranks high on the list of the most common causes of allergic reactions to food. This is not surprising when you take into account how extensively foods derived from this grain of choice are consumed in the typical American diet.
Consider how frequently popular food items made from wheat are eaten – everything from pizza, pasta, burger buns, and sandwich bread, to cereal, toast, pancakes, bagels and pastries - not to mention all of the snack and dessert items like crackers, pretzels, cookies, brownies, cakes, and pies. It is no wonder that health complaints, including digestive problems, stiff and painful joints, headaches, fatigue, brain fog and other conditions linked with wheat allergies and gluten sensitivity are so prevalent today.
The fact that grains are not the same today as they were hundreds of years ago is another reason that problems related to wheat and gluten consumption are increasing. The nutritional content of grains – especially wheat – has been altered by many generations of hybridization (cross breeding), as well as by many chemical processes used to ward off pests and diseases and meet the stringent demands for increased production and protein levels.  It is the proteins in wheat that trigger wheat allergies or sensitivity to gluten, and those proteins are present at higher levels than ever before.
It is the proteins in wheat that trigger wheat allergies or sensitivity to gluten, and those proteins are present at higher levels than ever before.
Just What is Gluten?
Gluten is a gum-like substance that forms when two proteins (glutenin and gliadin) found in the starchy portion of wheat and other grains come in contact with liquid. Gluten helps dough rise by providing the elastic bonds that trap bubbles of gas formed by the action of yeast or other leavening agents.  The longer you knead the bread during the bread-making process, the more elasticity is achieved by the gluten in the dough and the more the bread will rise. Without gluten, dough used for leavened bread would collapse and easily fall apart. Additionally, gluten firms up when cooked, giving bread its rigidity and chewy texture.
The longer you knead the bread during the bread-making process, the more elasticity is achieved by the gluten in the dough and the more the bread will rise. Without gluten, dough used for leavened bread would collapse and easily fall apart. Additionally, gluten firms up when cooked, giving bread its rigidity and chewy texture.
Although gluten is found most abundantly in wheat, grains such as barley, rye, spelt, kamut and tritricale contain it as well. Just because a food is “wheat free” does not necessarily mean it is “gluten free”. Oats don’t actually contain gluten, but since they are often processed and/or transported with wheat, they can easily become contaminated. Some form of gluten is used as a filler, extender or binding agent in many grainless foods and even non-food items.
It is important to realize that a wheat allergy is different from the type of food intolerance created by gluten. However, since avoiding gluten involves eliminating all forms of wheat, much of the information in this article can apply to both wheat allergies and gluten sensitivity. 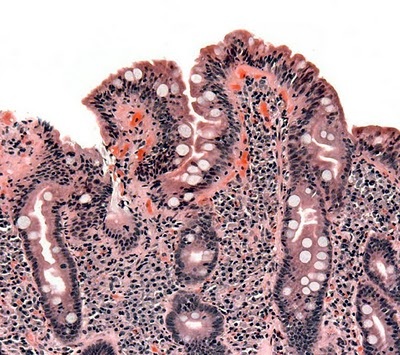 Understanding Celiac Disease
Understanding Celiac Disease
Celiac (pronounced “See’ lee ack) is a genetically linked digestive disease involving the immune system, which is triggered by an inability to digest gluten. With this disease, the body’s reaction to undigested gluten typically produces damage to the villi (tiny hair-like projections that absorb nutrients) in the lining of the small intestine. Without healthy villi, a person cannot obtain nutrients from their food.
A person with celiac disease lacks particular enzymes needed to digest one or more of the hard-to-digest proteins that make up gluten. The presence of these proteins in the digestive tract triggers an inflammatory immune response in which antibodies are formed against that protein. High levels of these antibodies in the blood are a common indicator of celiac. If symptoms suggest the possibility of celiac and a blood test reveals high levels of these antibodies, tissue samples are then taken from the small intestine to be biopsied. If the biopsy reveals damage to the intestinal villi or other characteristics of celiac, a diagnosis is made.
Just 20 years ago, celiac disease was regarded as a rare condition, affecting only approximately 40,000 Americans. Now it is believed that as many as one in a hundred, or nearly 3 million, people in the United States suffer from it, although only about 3% of existing cases are clinically diagnosed.
Beneath the Tip of the Gluten Iceberg
The small percentage of people with a classical clinical diagnosis of celiac represents just the tip of the iceberg of people significantly affected by gluten. “Silent celiac” is another form of the disease discovered in recent years. In this condition, damage to the villi occurs, but the obvious symptoms are absent, meaning it is rarely diagnosed.
Latent celiac is yet another form that is even less recognized. With this type of celiac, a person’s antibody tests are positive, but there seems to be no damage to the small intestine, so they may be advised by conventional medical doctors to continue eating gluten. Symptoms worsen, and these people eventually develop full-blown celiac.
The base of the iceberg represents people who carry genetic susceptibility to celiac disease, referred to as “gluten sensitivity.” These people have a degree of sensitivity to gluten and experience symptoms, although the connection with gluten is generally not made. According to research conducted by Dr. Kenneth Fine, an internationally recognized gastrointestinal specialist and founder of the Intestinal Health Institute, as many as 50% of the population may be gluten sensitive.
What Symptoms Can Gluten Cause?
The number of symptoms related to gluten intolerance or celiac disease is estimated by some sources to be as high as 250. Not surprisingly, many of these symptoms overlap with other diseases and conditions.
In children, the most common symptoms related to gluten are abdominal pain and bloating, poor appetite, diarrhea, or chronic constipation. Due to the lack of nutrient absorption, malnutrition, weight loss, stunted growth and delayed puberty may also occur. Celiac is also thought to be connected with autism and conditions related to learning and behavioral disorders.
In addition to similar gastrointestinal disorders, adults tend to have some or some combination of the following symptoms: fatigue, headaches, unexplained weight gain, anemia, mouth ulcers, skin rashes, joint/bone pain, seizures, infertility or recurrent miscarriages. Continued damage to the small intestine makes it more likely that gluten-related health problems like early-onset osteoporosis, thyroid abnormalities or autoimmune diseases will develop.
Since symptoms of other physical disorders are often similar to those caused by gluten intolerance, celiac or gluten sensitivity is often overlooked, misdiagnosed or easily confused with such conditions as irritable bowel syndrome, iron-deficiency anemia caused by menstrual blood loss, diverticulitis, Crohn’s disease, intestinal infections, or chronic fatigue syndrome.
Gluten is also one of the irritants that can lead to a “leaky gut” condition, which allows undigested proteins to enter the bloodstream. As I covered in Part 2 of this series, undigested proteins entering the bloodstream is a primary way for other food allergies (and their attendant symptoms) to develop.
The Importance of Discovering if You Are Gluten Sensitive
Until recently, it took about 11 years to accurately diagnose a person suffering with celiac disease. By that time, significant intestinal damage and the development of other related physical conditions may have occurred. Fortunately, the speed at which this diagnosis is reached is increasing as testing methods become more reliable and doctors become more aware of the latest scientific research and findings regarding this disease.
 If you at all suspect that eating wheat products bothers your system, it is extremely important to discover whether or not you are gluten sensitive, because severe health complications can result from continuing to eat gluten if sensitivity exists.
If you at all suspect that eating wheat products bothers your system, it is extremely important to discover whether or not you are gluten sensitive, because severe health complications can result from continuing to eat gluten if sensitivity exists.
A study published last year in the Journal of the American Medical Association (JAMA), involving 30,000 patients over a forty year period (1969-2008), found that serious consequences from eating gluten occur even when there is no diagnosis of celiac disease. In addition to those diagnosed with celiac, two other groups were included in the study: those who had experienced any gluten-based intestinal inflammation and those who had elevated gluten antibodies but no evidence of intestinal inflammation or damage (latent celiac disease.)
An increased risk of death occurred in all three groups, primarily from heart disease and cancer. Those with intestinal inflammation who were not diagnosed with celiac had a significantly higher percentage (72%) than the other two groups (39% for those with celiac and 35% for those with gluten sensitivity or latent celiac disease).
The longer a person with gluten intolerance goes without being diagnosed or treated, the greater the chance of developing long-term complications.
Another study (Gastroenterology – April, 2009) led by a team of Mayo Clinic doctors and scientists confirmed the long-term health consequences of undiagnosed gluten sensitivity. That study also revealed the extent to which this disease is increasing. It involved analysis of blood samples first taken from 9,333 of healthy young adults between 1948 and 1954, contrasted with blood samples from a test group of 12,768 comparable individuals. Undiagnosed celiac disease was associated with a nearly four-fold increased risk of death. The study also concluded that rates of undiagnosed celiac disease have increased dramatically in the United States over the last 50 years.
The Only Remedy – a “Gluten-Free” Diet
Whether a person has full blown celiac disease, or just experiences symptoms from gluten sensitivity, eating a gluten-free diet is the only remedy that works. A strict gluten-free diet prevents further damage and resulting nutritional deficiencies, while healing existing damage so that nutrients may once again be absorbed.
If you suspect you might have celiac disease and want to be tested, you should do so before beginning a gluten-free diet. One reason for this is that antibody blood tests may not be accurate or useful if gluten is not consumed during the period of testing. Obtaining a gluten sensitivity stool test is another laboratory testing option that is believed to detect cases of gluten sensitivity earlier in the disease process. With this test, you continue with the same diet and do not have to resume eating gluten if you have already removed it from your diet. You can learn more about this type of testing and order the test from Enterolab.
For those who are not completely certain if they need to avoid all gluten, Dr. David Brownstein recommends in his book, The Guide to a Gluten-Free Diet going on a six week “therapeutic trial” to see if symptoms improve. The reason he suggests this period of time is that the immune system can still react to gluten up to six weeks after it is ingested, due to its cumulative effect.
The Challenge of Avoiding Gluten
Eating gluten-free in today’s society is extremely challenging, not to mention socially inconvenient. It involves more than just avoiding breads and pasta made with gluten grains. The number of food and non-food products containing gluten is surprising and can be overwhelming for those who need to avoid every trace of the substance.
Since gluten is used as a thickener and extender in a number of processed foods, gluten-sensitive people should carefully check the ingredient labels of food items, such as:
- Soups

- Bouillon cubes
- Sauces (Barbeque sauce, soy sauce)
- Gravy
- Salad Dressings
- Cereals
- Snack foods (seasoned chips, potato chips)
- Desserts/candy
- Cold cuts, hot dogs, salami, sausage
- Flavored instant coffee and teas
- Dairy products (ice cream, yogurt, blue cheese, coffee creamers)
- Seasoning and flavoring products (MSG)
- Rice mixes
- Hydrolyzed plant or vegetable protein (HPP or HVP)
- Textured plant or vegetable protein (TPP or TVP)
- Modified food starch
- Caramel coloring
- Rice syrup or malt (contains barley)
- Dextrin, malt, maltodextrin
- Communion wafers
- Imitation fish
If the ingredients are not listed on the label, the manufacturer should provide a list upon request.
In addition to rye, barley, triticale (cross between wheat and rye) spelt, and kamut, all forms of wheat should be avoided including wheat starch, wheat bran, wheat germ, cracked wheat, bromated flour, durum flour, enriched flour, graham flour, farina, semolina, and self-rising flour.
Besides avoiding these foods and ingredients, individuals sensitive to gluten need to be aware that personal care and other non-food products may also contain traces of gluten, which can be absorbed into the body through the skin. This would include certain kinds of lotions, soaps, hair products, lip balm, toothpaste and mouthwash. Glue on stamps and envelopes, chewing gum (sometimes dusted with wheat starch) and even some kinds of medications or supplements can contain wheat or gluten as wheat starch is commonly used as a binding agent in tablets and capsules.
Making the Transition to a Gluten-Free Diet
While you are making the transition to “gluten-free” living, it may be helpful to carry with you a list of foods you can eat and foods you should avoid. If in doubt about any product, check with the manufacturer to be on the safe side, especially if you are highly sensitive. Of course, a good way to be safe and avoid cross contamination is to either buy items that are certified “gluten-free” or to purchase gluten-free ingredients and prepare foods yourself. Avoiding processed foods and sticking to a diet of plainly prepared meat, fish, poultry, beans, legumes, eggs, dairy, nuts, seeds and other “allowed” foods is the simplest and healthiest option for staying gluten free.
Because of the increase and awareness of gluten and wheat allergies, finding options for gluten free baked goods, pasta, cereals, snack items, etc. is not as difficult as it once was. Besides health food stores and food co-ops, many of the larger chain grocery stores have a “gluten-free” section or at least carry gluten free items. If you have no access to any of these options, gluten free foods may even be ordered online on sites such as http://www.glutenfreemall.com and http://www.amazon.com.
One word of caution when selecting gluten free products – just because it is gluten free does not necessarily mean it is healthy. Many times gluten free baked goods and snack items are as refined and void of fiber as their white flour counterparts. They may also be high in sugar and contain hydrogenated oils and other unhealthy ingredients. Getting gluten out of your diet may help in one sense yet cause other types of health issues in another if a person is eating processed foods with sugar, bad fats and too much starchy refined flour.
What to Use in Place of Gluten Flours
A variety of flour substitutes can be made from non-gluten grains, seeds, nuts, legumes and vegetables to use in recipes. These alternatives for gluten flour work best when used in combination. Some of the more common ones used in gluten free cooking and baking are: 
- Rice (brown rice flour is best)
- Millet
- Almond
- Flaxseed meal
- Buckwheat
- Garfava (made from garbanzo and fava beans)
- Quinoa
- Coconut
- Amaranth
- Tapioca
- Arrowroot
- Potato
- Cornmeal
- Sorghum
- Teff
Flours made from beans, seeds, nuts, coconut and grains like quinoa and amaranth are healthier options in that they contain higher levels of protein and fiber, whereas potato, tapioca and white rice flour are starchier with little fiber. 
Depending on what you are making, however, you may need a certain amount of the “white” starchier flours to keep the product from being too “heavy”, which is why a combination of flours is recommended for gluten-free baking. You can either make your own “baking mix” using a blend of different flours or enjoy the convenience and ease of gluten-free baking mixes that are pre-mixed to provide consistent results with various types of recipes.
When baking or cooking without gluten, it is necessary to use some type of binding agent to serve as a gluten replacement. Using ½ to 1 teaspoon of xantham gum (a fermented corn-based thickener) per cup of gluten-free flour in baking recipes is highly recommended. Other options are guar gum (from the seed of a bean-like plant with eight times the thickening power of cornstarch) or arrowroot powder (an unrefined thickener from the roots of a South American plant) that may be used in similar amounts. Using extra eggs as a binding agent is another option if you wish to avoid more starchy substitutes.
 Tips and Support for Gluten Free Living
Tips and Support for Gluten Free Living
A wealth of information may be obtained from numerous sources for anyone who must avoid gluten or who has a child or other loved one with gluten intolerance. As an example, Dr. David Brownstein’s book The Guide to a Gluten-Free Diet (2nd edition – 2009), contains many helpful tips for living gluten-free including:
- How to handle the challenges of eating away from home
- Ways to avoid cross-contamination when preparing foods and eating out
- Ways to get more nutrition on a gluten-free diet
- Gluten free meal and snack ideas
- How to handle having a gluten sensitive child
Many wonderful recipes are included that were created by the co-author of the book, Sheryl Shenefelt, a certified nutritionist. Books by Dr. Brownstein, Medical Director of the “Center for Holistic Medicine”, may be obtained through his website http://www.drbrownstein.com
The following websites also provide a great deal of helpful information and support:
- http://www.celic.com (to find support groups as well as articles, recipes and other helpful resources)
- http://www.livingwithout.com (lifestyle guide for people with allergies and food sensitivities)
- http://www.glutenfreeliving.com (magazine providing guidance and support to those transitioning to a gluten-free lifestyle)
- http://www.glutenfreeda.com (online cooking magazine for people with celiac and gluten sensitivity)
- http://www.glutenfreebakingandmore.com (gluten-free baking and cooking ideas, product reviews, etc.)
- http://www.glutenfreerestaurants.org (find restaurants in your area that serve gluten-free foods)
If you have any unresolved health complaints or difficulty losing weight, you may want to experiment with eliminating grains for a period of weeks and see if you notice any improvements. Even if you do not have celiac disease or any particular sensitivity to gluten that you are aware of, everyone could benefit health-wise (as well as weight-wise) by reducing the amount of grains, especially wheat, in their diet.
Next month's focus:
Proteins in milk may cause allergic reactions in people much the same as those produced by gluten. The last in this series of food allergy articles will focus on allergies and sensitivities to milk and other dairy products and provide help for those who may need to go "dairy-free".
Sources:
- The Guide to a Gluten-Free Diet by David Brownstein, M.D. and Sheryl Shenefelt, C.N.
- Going Against the Grain by Melissa Diane Smith
- Ultrametabolism by Mark Hyman, M.D.
- http://www.bcm.edu/gastro/DDC/grandrounds/UT/8-12-04/09-DISC.HTM
- http://glutenfreecooking.about.com/od/glutenfreecookingbasics/a/xanthanguargums.htm
- http://bakingdesserts.suite101.com/article.cfm/wheatfree_glutenfree_baking
- http://www.againstthegrainnutrition.com/newsandnotes/2010/01/08/undiagnosed-gluten-sensitivity-andceliac-disease-increase-risk-of-death/
- http://digestive.niddk.nih.gov/ddiseases/pubs/celiac/
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||


