| Share |  |
 | |||
Better Bone Health - Solutions for Osteoporosis - Part 2
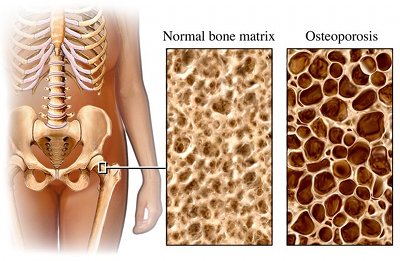 Improving the health of the bones involves much more than the typical solutions often given for preventing or correcting osteoporosis – drinking more milk, eating more dairy products and taking calcium supplements or osteoporosis drugs. The reason is that osteoporosis is not as much about the weakening of the bones as it is about factors related to deterioration occurring throughout the body.
Improving the health of the bones involves much more than the typical solutions often given for preventing or correcting osteoporosis – drinking more milk, eating more dairy products and taking calcium supplements or osteoporosis drugs. The reason is that osteoporosis is not as much about the weakening of the bones as it is about factors related to deterioration occurring throughout the body.
If bones are to become healthy, the whole body must be treated by addressing and reversing the underlying causes of the disease process. Medications will not fix imbalances in the body that took years to develop. The good news is that discovering the hidden factors involved in bone loss and taking the needed measures to build stronger bones will greatly benefit overall health.
Understanding Root Causes
As is common with many of the degenerative diseases people experience today, chronic low levels of inflammation is a primary root issue underlying bone deterioration and the ability of bones to rebuild and repair. Though drugs may harden bones, they do not stop chronic inflammation or fix the actual mechanism responsible for the loss of bone mass.
Chronic inflammation is more subtle than acute inflammation, 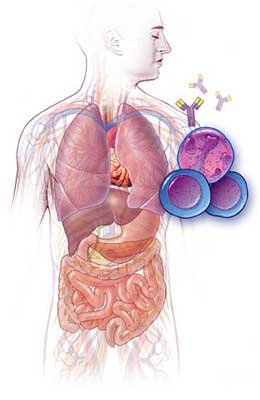 which is characterized by obvious redness, heat, swelling, and pain. The problem occurs when immune cells are activated on an ongoing basis and inflammation becomes systemic, meaning any system in the body may be impaired. When the skeletal system is affected, ongoing inflammation disrupts the balance between bone breakdown and bone growth and interferes with chemical signals that tell the osteoclasts (cells that break down bone) to cease their activity. As these cells survive beyond their normal lifespan, bone breakdown surpasses bone build-up.
which is characterized by obvious redness, heat, swelling, and pain. The problem occurs when immune cells are activated on an ongoing basis and inflammation becomes systemic, meaning any system in the body may be impaired. When the skeletal system is affected, ongoing inflammation disrupts the balance between bone breakdown and bone growth and interferes with chemical signals that tell the osteoclasts (cells that break down bone) to cease their activity. As these cells survive beyond their normal lifespan, bone breakdown surpasses bone build-up.
Oxidative damage from free radical activity is a further root cause of disease that takes place along side of inflammation. The more oxidative stress, the more free radicals are produced. The more free radicals are produced, the more damage takes place in tissues and the greater the body’s inflammatory response. This becomes a perpetuating vicious cycle as chronic inflammation within the tissues produces more and more oxidative stress, which then creates more inflammation – the end result of which is a progressive accumulation of tissue damage and bone loss. Free radical activity is generated by diets deficient in anti-oxidants and high in sugar, bad fats, fried foods, excess meats and processed foods, in addition to unhealthy lifestyle habits, toxins and environmental factors.
Good Digestion and  Gut Health – A Must for Healthy Bones
Gut Health – A Must for Healthy Bones
Bone health is dependent upon the absorption of nutrients. Problems in the digestive tract not only prevent the assimilation of nutrients essential for strong bones but also contribute to the underlying roots of inflammation and oxidative stress. Eliminating gastrointestinal stress, which leads to systemic inflammation, allows the body to absorb critically needed nutrients for bone health.
One reason for poor digestion is the lack of sufficient digestive secretions, namely enzymes and stomach acid. Having low levels of hydrochloric acid, or neutralizing stomach acid by taking antacids, acid blockers, or certain types of calcium is problematic on several counts. For one thing, it removes the needed protection from any harmful bacteria entering the body that would pass through the stomach and into the intestines and bloodstream. In addition, proteins and minerals cannot be adequately broken down for proper assimilation without ample levels of hydrochloric acid. The great majority of poor absorption of calcium and other minerals is due to low levels of hydrochloric acid in the stomach. It is estimated that half of people over the age of 60 have insufficient amounts of hydrochloric acid, as production can slow with age.
While hydrochloric acid is working on breaking down foods, the stomach pH is reduced to a very acidic pH level as low as two. Once the food is thoroughly transformed into chyme, hydrochloric acid production decreases and the pH level of the stomach rises. This signals the body to open the sphincter that allows the food to leave the stomach and enter the small intestine. If antacids, acid blockers or calcium carbonate is taken, hydrochloric acid is neutralized or blocked, which means the stomach pH rises prematurely. In this case, the signal is sent that digestion in the stomach is completed even though the food is not thoroughly broken down.
When food is not properly digested in the stomach, molecules of partially digested food enter the small intestine. These undigested food molecules create acids and provide material for microbes such as yeast and bad bacteria to feed on, which allows them to proliferate. The overgrowth of microbes contributes to malabsorption, gut inflammation and eventually bone loss.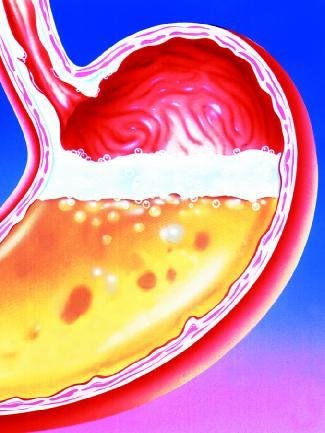
Inflammation from undigested food molecules, along with the acids produced from the overgrowth of yeast and bad bacteria, cause gaps to form amidst the normally tight juncture of cells in the intestinal wall. What is commonly known as “leaky gut” develops, a condition that allows larger incompletely digested food molecules to escape into the bloodstream. The presence of these molecules in the bloodstream prompts the body to turn on its defenses and mount an immune response.
Once a food allergy or sensitivity has developed and that food continues to be ingested, the immune system is kept on high alert. Further inflammation is produced from the ongoing irritation to the intestinal tract lining, which worsens leaky gut syndrome. As the inflammation becomes systemic, levels of pro-inflammatory chemical messengers increase, activating an over production of the type of cells that break down bone. This throws the normal bone remodeling process out of balance.
Disease of Calcium Deficiency or Calcium Loss?
When people think of bone health, they tend to just think of the need to obtain more calcium. Although calcium is a major component of bones and essential for bone strength, bone and bone tissue is made up of many other minerals (magnesium, phosphorus, sodium, potassium, zinc, uranium, plutonium and strontium), connective tissue proteins (collagen, silica), enzymes and molecules called cytokines. Minerals give density to bones and supply the rigid structure, but it is the protein matrix consisting of collagen and connective tissue that give bones their strength and resilience. Without sufficient amounts of these other elements, healthy bones cannot be created no matter how much calcium a person takes. Rather than not enough calcium, poor bone health is more due to general lack of good nutrition, especially trace minerals.
Plus taking too much calcium can produce relative deficiencies of other nutrients important for bone health, such as magnesium, and vitamins D and K. It can also lead to too much “free” or unbound calcium in the blood. Excess amounts of unbound calcium that is not absorbed into the bone can cause kidney stones, bone spurs, gallstones, increased plaque on teeth and calcifications in coronary arteries that lead to the build-up of arterial plaque and increased risk of heart disease.
The Real Cause of Calcium Depletion
It is important to remember that the calcium in bones, which represents approximately 99 percent of total body calcium, remains fairly consistent as long as the body is in a healthy state. Rather than lack of sufficient calcium intake accounting for deteriorating bones, the question that should be considered is “what is causing calcium to be depleted from the bones?”
Since calcium is the main alkalizing mineral in the body, the primary reason it is withdrawn from the bones is to rebalance blood pH levels. For a person to stay alive, the acid/alkaline balance of the blood must be maintained within a very narrow range. Survival then takes precedence over bone health in the priority levels of the body.
An acidic environment accelerates the rate at which osteoclasts dissolve bone tissue and halts the production of new bone by the osteoblasts. Levels of the growth hormone IGF-1 are also greatly reduced when the body is acidic (IGF-1 stimulates production of cartilage and bone as well as calcium absorption, bone production and mineralization). When the body must compensate for an acidic pH over a prolonged period of time, osteopenia or osteoporosis often results. Supplementing with calcium will not begin to offset the damage to the bones caused by a high acid forming diet. How does the body become acidic? Quite simply, it is from consuming too many acidic foods and beverages (meats, grains, dairy products, sugar, refined carbohydrates, soda, coffee, etc.) and too little alkalizing fruits and vegetables.
Effects of Toxins and Metals on Bone Health
Although I have covered the major underlying causes of osteoporosis, additional factors that can account for bone loss may need to be considered as well. Increasing amounts of environmental toxins and chemicals in today’s world are a further cause of inflammation that contributes to chronic disease. Toxic metals in particular interfere with vitamin D metabolism and otherwise hinder the normal processes involved in healthy bone building. The worse offenders are:
Aluminum – aluminum follows the absorption and deposition pathways of calcium (low calcium levels increase amounts of aluminum absorbed) and is known to cause extensive bone disease, as evidenced by kidney dialysis patients who received dialysis fluids containing high levels of aluminum. When aluminum is absorbed, it interferes with bone cell activity and hydroxyapatite crystal formulation, which leads to lower bone density and increased fracture risk. Aluminum is absorbed most frequently from antacids, baking powder, deodorants, aluminum-containing cookware, foil, processed foods and contaminated water sources.
Lead – lead disrupts enzyme function and reduces the ability of osteoblasts to form bone. Ingested or inhaled lead competes with calcium for absorption and is deposited into bone where it tends to accumulate over time. Even exposure to lead as a child could become a problem later as it may be released into the blood and cause loss of bone density during intense times of bone remodeling, such as menopause. Blood tests do not show amounts of lead sequestered in the bones.
Cadmium – Many studies have revealed how exposure to cadmium results in lowered bone density and fracture rates. Besides increasing oxidative stress and inflammation, this metal disrupts vitamin D production in the kidneys, limits the osteoblasts cell formation of bone collagen, and reduces progesterone and blood calcium levels. People may be exposed to cadmium through shellfish, canned foods, fish from polluted rivers, cigarette smoke, car exhaust and exposure to nickel-cadmium battery manufacturing.
Mercury – the role of mercury in osteoporosis is not clearly established but it is known to increase oxidative stress, deplete antioxidants, lower zinc levels needed in critical enzyme actions and interfere with the effectiveness of progesterone and other hormones. The primary sources of mercury are fish (both fresh and saltwater), dental amalgam fillings and thimerosal, a preservative in vaccines.
Iron – while not a toxic metal, excessive iron increases the production of free radicals, which creates more oxidative stress. Studies indicate that iron overload suppresses bone formation and stimulates bone resorption. The recommendation is not to take iron supplements if you are postmenopausal unless blood tests clearly show a need.
You may learn more information with regard to signs and symptoms, testing and therapies for heavy metal toxicity in The Whole-Body Approach to Osteoporosis by Dr. R. Keith McCormick. Other forms of toxicity that can affect bone health are:
Medications – Common medications associated with bone loss and increased risk of bone fractures are antidepressants, convulsants, sedatives, sleeping pills, steroids, SSRI antidepressants, Coumadin (known to l ower vitamin K levels by 65% in osteoporosis subjects) and long term antacids.
ower vitamin K levels by 65% in osteoporosis subjects) and long term antacids.
Fluoride – Fluoride, which is commonly found in tap water, toothpastes and mouthwashes, consists of hydrofluoric acid that is a chemical by-product of aluminum, steel, cement, phosphate, and nuclear manufacturing. While fluoride has been used in the treatment of osteoporosis, it actually disrupts the formation of enzymes necessary for collagen production and interferes with mineralization of bones and teeth. It also causes low blood calcium by taking calcium out of solution, which allows it to build-up and become calcium stones and crystals in the joints and organs. A definite correlation between fluoride and hip fractures in elderly women is borne out by many studies.
Stress – while not a toxin per se, stress contributes to inflammation and causes excess production of cortisol by the adrenal glands. When cortisol levels are constantly elevated, it impairs the function of bone-building cells and results in lowered bone mineral density and increased fracture risk.
The Role of Hormones in Bone Health
Before we explore all the many ways to improve bone health through diet, supplements and exercise, it is important to understand the important role hormones play in maintaining the mineral balance of the bones. Many factors can contribute to reduced or erratic hormone production, including age, poor health, chronic inflammation, toxic exposure, and gastrointestinal dysfunction. Though it is beyond the scope of this article to delve into how all of these naturally produced chemicals work in the body to influence bone health, I have listed and briefly described the primary ones that may be out of balance when a person has osteoporosis.
The following three hormones work together in different ways to regulate calcium and bone mineral balance in response to reduced blood levels of calcium.
Parathyroid hormone – is the primary regulator of blood calcium levels. It works by limiting the excretion of calcium by the kidneys through the urine, activating vitamin D levels that facilitate calcium absorption from food, and stimulating the process of bone remodeling to jumpstart the release of calcium into the bloodstream.
Calcitriol – is the hormonal form of vitamin D that increases intestinal absorption of calcium and stimulates osteoblasts to form bone. This active form of vitamin D also acts as a feedback mechanism to signal the parathyroid glands to stop releasing parathyroid hormone.
Calcitonin – is a hormone secreted by the thyroid gland that promotes the transfer of calcium to the bone by inhibiting the breakdown of bone by the osteoclasts.
The following reproductive hormones are involved in the regulation of bone loss.
Estrogen – a form of estrogen, known as estradiol, is vital for skeletal health as it works to temper the breakdown of bone in addition to increasing calcium absorption and stimulating osteoblasts (bone-building cells). Since estrogen is a regulator of calcium, low levels can prevent the absorption and utilization of calcium. This leads to osteoporosis, which explains why post-menopausal women are more likely to develop osteoporosis. Women with low body fat are particularly susceptible since fat is essential to maintaining estrogen levels. Hot flashes, night sweats, vaginal dryness, memory loss, sleep disturbances, and frequent urination are a few of the signs of low estrogen levels.
Progesterone – progesterone is thought to work in two ways to improve bone health - first by stimulating bone collagen formation and, secondly, by blocking the adrenal gland hormone cortisol which has a harmful effect on bone density. High levels of cortisol that often result from prolonged stress reduce the body’s ability to make progesterone. Anxieties, mood swings, sleep disturbances, irritability, depression and irregular or heavy periods are some of the signs of low progesterone in women. Natural progesterone increases bone strength and density by stimulating osteoblasts, the bone building cells. If progesterone levels are low, a natural plant-based progesterone cream or bioidentical hormone compound can restore levels and improve bone health.
Testosterone – low testosterone levels in men are associated with low bone density but the associated elevated fracture risk appears be due to the lower levels causing increased systemic inflammation. Low levels of both estrogen and testosterone increase inflammation and are linked to osteoporosis in both men and women.
This final group of hormones is necessary for maintaining growth and metabolic balance.
IGF-1 (insulin-like growth factor) – is a hormone produced and released by the liver. Deficient levels, made worse by chronic inflammation, lead to osteoporosis and low muscle mass.
DHEA – is the mother hormone to estrogen, progesterone and testosterone, which is considered a biomarker of aging. Low DHEA levels lead to reduced production of reproductive hormones, such as estrogen, and are associated with osteoporosis.
Cortisol – reduces the ability of the osteoblasts to form bone which is why chronic stress and elevated cortisol levels are associated with reduced bone density and increased fracture risk.
Thyroid hormone – overproduction of the thyroid-stimulating hormone (TSH) leads to bone loss as well as increased production of pro-inflammatory molecules that create systemic inflammation. Either hyperthyroidism or too much thyroid medication may cause this condition.
Osteocalcin – is a protein secreted by osteoblasts (bone-building cells), which also acts as a hormone that helps regulate metabolism by causing beta cells in the pancreas to release more insulin. Osteocalcin is heightened by potassium, vitamin K, berberine (an herbal alkaloid) and any supplemental or dietary measures that increase alkalinity and reduce inflammation.
Serotonin and melatonin – 95% of what the body produces in the way of serotonin is produced in the gut. Gut inflammation causes serotonin levels to rise, which compromises serotonin reuptake mechanisms and allows for the build-up of serotonin. Excess serotonin filters into the blood and ends up in the bones where it inhibits bone formation. Large amounts of melatonin are produced within the bone and foster osteoblast cell formation. Adequate melatonin levels from restful and regular sleep limit excessive production of serotonin. For a more complete discussion about these hormones and natural ways to restore balance when they are deficient or excessive, I would encourage you to read the chapter “Your Body’s Regulatory Hormones: the Pulse of Skeletal Health” in Dr. McCormick’s book The Whole-Body Approach to Osteoporosis. While hormone replacement may be beneficial in some cases, Dr. McCormick is quick to point out that it is by no means a “miracle cure”, especially if the root issues of nutritional deficiencies, poor gastrointestinal health or toxic overload are not first addressed.
McCormick’s book The Whole-Body Approach to Osteoporosis. While hormone replacement may be beneficial in some cases, Dr. McCormick is quick to point out that it is by no means a “miracle cure”, especially if the root issues of nutritional deficiencies, poor gastrointestinal health or toxic overload are not first addressed.
Dietary Guidelines for Improving Bone Health
In order to get adequate amounts of protein, minerals and collagen needed for healthy bone formation and repair, the emphasis should be on consuming more whole unprocessed, alkalizing foods rather than just taking supplements. Though by no means complete, the following lists will give you some general ideas about what is best to consume, what items should be limited or perhaps avoided altogether if you want to prevent or reverse osteoporosis.
WHAT TO CONSUME
Omega-3 fats and healthy oils – Eating more foods that are rich in omega-3’s can be one of the easiest ways to offset the effects of inflammation on your bones. Examples of food sources high in omega-3 are wild caught cold-water fish (especially salmon), sardines, flaxseeds, flaxseed oil, walnut oil, nuts (walnuts, almond, hazelnuts, pecans, etc.) avocados, dark green leafy vegetables and grass-fed beef (contains two to four times more omega-3 than conventional grain-fed beef). Organic butter, extra virgin coconut oil and olive oil are best to use for cooking.
Nutrient-dense alkaline foods – Consume plenty of fresh or freshly frozen fruits and vegetables (organic produce contains far more minerals and other nutrients and is free from chemical toxins, irradiation, etc.) - five to nine servings of fruits and vegetables each day will help alkalize the body and lessen the bone-robbing effects of the typical acid American diet.
Quality sources of protein –At least 30 percent of the diet should consist of quality protein, which is essential to build and repair tissue. Animal sources of protein, complete with all of the essential amino acids, are especially important to build the protein matrix used in bone formation. Quality proteins consist of wild-caught seafood and gras s-fed lean poultry and beef, and free range eggs. Although animal protein is beneficial in stimulating IGF-1 (insulin growth factor) that triggers bone growth and mineralization, it is important to eat smaller amounts at a time balanced with plenty of alkaline foods to maintain proper pH levels since meat is acidic.
s-fed lean poultry and beef, and free range eggs. Although animal protein is beneficial in stimulating IGF-1 (insulin growth factor) that triggers bone growth and mineralization, it is important to eat smaller amounts at a time balanced with plenty of alkaline foods to maintain proper pH levels since meat is acidic.
Bone broth - Eat soups made with lots of vegetables and bones from chicken or beef that will add many of the minerals and other nutrients needed for bone health. Adding one tablespoon of vinegar to every eight cups of water helps to extract the calcium and other minerals from the bones and into the broth of the soup.
Foods high in bone-building nutrients –broccoli, dark green leafy greens, seeds (pumpkin and sesame), nuts (especially almond) legumes, onions, prunes, oranges, cultured dairy products (preferably from goat’s milk and organic sources) and seafood such as salmon and oysters.
WHAT TO AVOID
Sugar and refined carbohydrates – Sugar robs the body of minerals and upsets the mineral balance needed for enzymes hormones to function effectively. Sugar depresses phosphorus levels, which causes a rise in levels of parathyroid hormone. This action then results in the excretion of phosphorus and magnesium needed to bind calcium into the bone. In addition, consuming sugar causes the release of insulin from the pancreas, which lowers levels of IGF-1 needed for bone health. Sugar is also very acid producing in the body, which accelerates the depletion of calcium from the bones. Refined carbohydrates (breads, pasta, white rice, etc.) quickly turn to sugar in the bloodstream and create similar effects.
Bad Fats - trans fats, hydrogenated or partially hydrogenated oils and all omega-6 vegetables oils (corn, soybean, safflower, sunflower, etc.) and the food products containing them (margarine, salad dressings, and all commercially produced baked goods and snack foods) significantly increase inflammation and damage the cell membranes
Processed foods – besides the fact that these foods are very nutrient deficient, the chemical additives, flavorings and preservatives they contain are toxic  to the body and therefore contribute to inflammation. The amount of nutrients needed by the liver to break down these chemicals adds to nutrient deficiencies in the body.
to the body and therefore contribute to inflammation. The amount of nutrients needed by the liver to break down these chemicals adds to nutrient deficiencies in the body.
Table salt and processed foods that are high in salt – commercial table salt is refined, bleached and highly acidifying to the body. On the other hand, unrefined sea salt contains many of the trace minerals missing from foods, is alkalizing and very beneficial for health.
Soft drinks, canned juices – these drinks are too high in phosphoric acid that depletes calcium in addition to being high in sugar.
Gluten or other possible food allergens - recent studies indicate a direct relationship between gluten reactivity and severity of osteoporosis. Reactions to gluten on any level can trigger an inflammatory response that is ultimately detrimental to bones. Plus the damage produced to the small intestine hinders its ability to absorb nutrients. Since any food allergy or sensitivity can intensify inflammation, it would be beneficial to strictly eliminate any suspect foods for at least two weeks and notice how you are feeling. Then reintroduce the same food and see if any reaction occurs in the next day or two.
For more information about gluten allergies, I would recommend that you read my article "Food Allergies - Could Gluten Be Your Problem?"
WHAT TO LIMIT
 Caffeine – tends to be acidifying and can deplete calcium and accelerate the loss of bone at higher amounts.
Caffeine – tends to be acidifying and can deplete calcium and accelerate the loss of bone at higher amounts.
Grain-fed animal protein – because meats are high in uric and sulfuric acid that need to be buffered by the body, they should be limited to smaller portion sizes and consumed less frequently. Organically produced grass-fed beef is higher in anti-inflammatory omega-3 and other health producing nutrients.
Grains – even whole grains are acid producing in the body and high in inflammation-producing omega-6 fatty acids and low in anti-inflammatory omega-3 fatty acids. Modern hybridized wheat contains more sulfuric acid per gram than any meat.
Dairy products – dairy products from commercially raised cows (especially non-organic sources) should be eliminated or greatly reduced, especially if the person has difficulty digesting casein (the protein in milk), or is lactose intolerant. Dairy is more acid-producing in the body which can use up more calcium than what the body can assimilate from the milk or dairy product (see accompanying article on “Are Dairy Products the Best Source of Calcium?")
Recommendations for Supplementation
Since today’s foods are often deficient in nutrients (especially minerals), and people do not always get enough of the right types of foods in their diets, filling in the gaps with supplementation is virtually essential to make sure the body has what it needs to build healthy cells and achieve a balanced state of health. Keep in mind that it takes five to seven times the amount of nutrition to build and repair as it does to maintain health. Consequently, those who already have compromised bone health and mineral imbalances will need to incorporate a greater amount and variety of these supplements for a longer period of time to reverse a long-standing condition versus someone who is primarily concerned about maintaining good bone health.
Everyone could benefit from the suggested supplements in this first group. Besides helping to correct the underlying root causes of poor bone health, they can improve the overall health of the body.
Digestive Aids – plant-based digestive enzymes, herbs that naturally stimulate the body’s production of stomach acid or a supplement that contains betaine hydrochloric acid all can work to ensure food is broken down well enough to be absorbed. For more information on digestive enzymes and digestion in general, please read my article “The Key to Good Digestion”. For more information on normalizing levels of stomach acid, you may want to read my article “Stomach Acid – Too Much or Too Little?”
Probiotics – probiotics (friendly bacteria) correct the imbalance of bacteria in the gut by reinoculating it with beneficial microorganisms that are critical to the absorption of nutrients. I would recommend using a good probiotic supplement made from live active cultures of Lactobacillus, Bifidobacterium and other species and/or incorporate “living” foods like organic unsweetened yogurt, kefir, sauerkraut, and kimchee into your daily diet.
Multivitamin/mineral supplement – depending on the quality of the diet, some people may need to take a high quality multi-vitamin/mineral supplement for overall nutritional support.
Trace Mineral supplement – Due to the fact that today’s foods are grown in such mineral depleted soil, trace minerals are often missing from our diets. Taking a mineral supplement that provides 70 key trace minerals the body needs in a highly bioavailable colloidal liquid form is beneficial for bone building as well as balancing pH levels.
Green Drink – a good way to ensure that your body gets plenty of nutrients from greens, vitamins, minerals, live enzymes, etc. is to use a nutrient-dense, pH balancing green powder supplement that can be mixed in a drink or blender shake to cleanse, alkalize and rejuvenate the body.
Protein Powder – while not a supplement in pill form, consuming a high quality protein powder in a shake made from high quality whey, hemp or pea/rice protein is highly beneficial in building better bone health, especially when it is consumed right after exercise.
Anti-oxidants – to reduce oxidative stress and subdue inflammation, supplying the body with anti-oxidants helps to eliminate excess free radical activity. Vitamins C, Vitamin E, Alpha Lipoic Acid, N-acetyl Cysteine are a few of the anti-oxidants Dr. McCormick recommends in his book.
Omega-3 Essential Fatty Acids – taking fish oll or krill oil are the most potent means of supplying the body with the omega-3 fatty acids needed to combat inflammation and reduce bone loss. Krill oil is believed to be even more bioavailable than fish oil and contains a powerful carotenoid called astaxanthin, which is also considered a very powerful anti-oxidant.
Supplements Specific to Bone Health
Although there are many other nutrients important to bone health that may be deficient, the following ones are the most commonly recommended to support bone building.
Calcium - When considering ways to increase calcium intake, keep the following points in mind:
- Calcium carbonate is the least assimilable calcium and the one that is the most likely to contribute to "free calcium" index levels. It currently reads: Calcium carbonate should be avoided as it is the least assimilable calcium and the one that is the most likely to contribute to high “free calcium” index levels.

- Taking calcium alone suppresses magnesium absorption and creates magnesium deficiency. This is not recommended since magnesium is needed to deposit calcium into the bones. Natural foods have a ratio of two to eight-parts magnesium to one-part calcium. Since a person generally gets seven times more calcium in their diet than magnesium, adding more magnesium is a better choice to achieve greater calcium deposition to the bones.
- Although calcium is better absorbed from foods, if you do take a calcium supplement, it is best to use a more assimilable amino acid chelate or calcium citrate form. Dr. McCormick also recommends microcrystalline hydroxyapatite complex. His recommendations for amounts of calcium to supplement are 1200-1500 mg/day (in conjunction with taking his recommended amounts of magnesium – 600-750 mg/day to keep a balanced calcium/magnesium ratio).
- Using mineral-rich herbs high in calcium is an even more preferred way to supplement the diet with calcium, according to many natural health practitioners. Herbal CA and HSN-W are examples of herbal blends that contain herbs naturally high in calcium that are also rich in other minerals and nutrients (such as silica) that nourish and build bones as well as joints and connective tissue. Skeletal Strength, is a particularly effective combination that not only includes mineral rich herbs but also a combination of vitamins, minerals and digestive aids that work synergistically to support the skeletal system.
- Calcium is abundant in a wide variety of fresh foods, which is why it should not be necessary to supplement as much as certain other minerals if a person is eating a pH balanced diet consisting of whole, natural foods. Foods that are especially high in calcium are broccoli (especially stalks), sesame seeds, chia seeds, dark leafy greens, almonds, beans, quinoa, oranges, cultured dairy products and dried herbs.
Vitamin D – adequate vitamin D is needed to ensure calcium and phosphorus are absorbed and transferred to the bones for storage. A deficiency can elevate parathyroid hormone levels, which can lead to excessive breakdown of bones due to the stimulation of osteoclast  activity. Supplementing vitamin D in its active form D3 is recommended since not everyone gets sufficient exposure to the sun or is able to manufacture it effectively through this mechanism. Dr. McCormick recommends supplementing with 2,000 IU per day of Vitamin D3. Vitamin D is also found in foods such as egg yolk, liver and saltwater fish.
activity. Supplementing vitamin D in its active form D3 is recommended since not everyone gets sufficient exposure to the sun or is able to manufacture it effectively through this mechanism. Dr. McCormick recommends supplementing with 2,000 IU per day of Vitamin D3. Vitamin D is also found in foods such as egg yolk, liver and saltwater fish.
Magnesium – Magnesium is one of the most important nutrients in the body, which is particularly vital for energy production, nerve conduction, electrolyte balance and for the proper function of hundreds of enzymes. Magnesium allows calcium to transported and used throughout the body and is responsible for the production of the parathyroid and calcitonin hormones so important to bone health. Diets low in magnesium result in increased numbers of osteoclasts and higher bone resorption as depleted levels of magnesium cause bone growth to cease. Dr. McCormick recommends supplementing with 600-750 mg/day of magnesium and avoiding an oxide or carbonate form of magnesium. Foods high in magnesium are green leafy vegetables, animal protein, seeds, almonds, avocados, and figs.
Vitamin K – Vitamin K is known to limit calcium loss in the kidneys and is vital to activating the protein osteocalcin needed to calcify and strengthen bones. Deficiencies in vitamin K are associated with low bone density and increased fracture risk. Dr. McCormick recommends at least 200-500 μg/day for optimal osteocalcin activity but as much as 1mg/day for general support for those with osteoporosis. Foods high in vitamin K are green, leafy vegetables such as broccoli, brussel sprouts, collard greens, spinach, sauerkraut, natto and kimchee.
Gaining Bone Strength through Exercise
 Immobility or inactivity greatly reduces bone density and increases the risk of fragility fracture. The importance role exercise plays in building stronger bones cannot be overemphasized. The more the force of muscles pulls against the bones, the more bone remodeling and bone formation is stimulated, and the stronger the skeleton becomes. The fact that bone deposits extra calcium in areas that are stressed also means a reduced likelihood of fracture. Moreover, exercise decreases falls by improving balance.
Immobility or inactivity greatly reduces bone density and increases the risk of fragility fracture. The importance role exercise plays in building stronger bones cannot be overemphasized. The more the force of muscles pulls against the bones, the more bone remodeling and bone formation is stimulated, and the stronger the skeleton becomes. The fact that bone deposits extra calcium in areas that are stressed also means a reduced likelihood of fracture. Moreover, exercise decreases falls by improving balance.
Dr. McCormick recommends getting at least 15 to 30 minutes of exercise, three to four times a week that consists of both weight-bearing exercise and strength or resistance training. Weight bearing exercise involves activities like walking, jogging, dancing, stair-climbing, aerobics or anything that has the body moving against the resistance of gravity.
Since muscles and bones are so interdependent, strengthening muscles is essential for creating stronger bones, especially in light of the fact that muscle mass declines an average of five percent each decade after the age of thirty. Lean muscle tissue and fat make up the soft-tissues of the body, the growth of which is essential in stimulating bone formation. When there is a loss of muscle mass and tone, it indicates the body is in the state of breaking down. To counteract this destructive pattern, muscles must be strengthened. This signals bones to follow suit.
 Strength training involves moving the body against some form of resistance using free weights, resistance bands, weight machines or simply resisting your own weight by doing wall push-ups, abdominal crunches, squats and the like. According to Dr. McCormick, maintaining muscle mass is the best strategy for retaining bone health with age.
Strength training involves moving the body against some form of resistance using free weights, resistance bands, weight machines or simply resisting your own weight by doing wall push-ups, abdominal crunches, squats and the like. According to Dr. McCormick, maintaining muscle mass is the best strategy for retaining bone health with age.
Concluding Thoughts
Everyone can benefit from applying the dietary and natural health principles covered in this article regardless of the state of your bone density. By following the nutritional, supplemental and exercise recommendations provided, you can give your body what it needs to build strong healthy bones and keep from developing osteopenia or osteoporosis.
If you already have either of these conditions and are in need of more specific information concerning the next steps to take for reversing them, I would highly recommend that you obtain a copy of The Whole-Body Approach to Osteoporosis by Dr. R. Keith McCormick. In it you will find very specific guidelines and information about the different types of testing available that is specifically related to bone loss as well as general health, hormone levels and nutritional deficiencies. Of particular benefit to assessing and monitoring your own bone health are tests that measure bone resorption and bone formation markers to determine if low bone density is due to excessive resorption or inadequate bone formation. By knowing this information, you can more effectively take appropriate measures to restore the health of your bones and improve your overall health in the process.
Sources
The Whole-Body Approach to Osteoporosis by R. Keith McCormick, DC
http://www.betterbones.com/osteoporosis/top10myths.aspx
http://www.womentowomen.com/bonehealth/inflammationandbones.aspx
http://www.treelite.com/NF/2008/07/BoneHealth.pdf
http://articles.mercola.com/sites/articles/archive/2002/02/02/fluoride-safety-part-one.aspx
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||



