| Share |  |
 | |||
What Really Causes Heart Disease
 Even with all the efforts to lower fat intake and cholesterol levels over the last several decades, heart disease is still the leading cause of death in this country. This fact should especially concern women as one out of three die of some form of cardiovascular disease each year - far more than from all types of cancer combined.
Even with all the efforts to lower fat intake and cholesterol levels over the last several decades, heart disease is still the leading cause of death in this country. This fact should especially concern women as one out of three die of some form of cardiovascular disease each year - far more than from all types of cancer combined.
People are led to believe that keeping cholesterol levels low will reduce their risk for heart attacks and strokes. The fact that the cholesterol levels of the majority of people who die of cardiovascular disease are within normal ranges challenges the validity of this notion. Lowering cholesterol with drugs may result in lower numbers but does very little to reduce underlying risk factors of heart disease. The real question that needs to be answered is, “what caused cholesterol levels to rise in the first place?” The most up-to-date research reveals that high cholesterol levels point to the presence of far more serious un derlying issues of health. Dealing with the root issues behind those health concerns will not only normalize cholesterol levels but will also greatly reduce the risk of other chronic diseases.
derlying issues of health. Dealing with the root issues behind those health concerns will not only normalize cholesterol levels but will also greatly reduce the risk of other chronic diseases.
The Underlying Root of Heart Disease
Although cholesterol is not what causes heart disease, it is actually used by the body as part of the solution to damage caused by the real problem. As was pointed out in last month’s article on “Exploring the Cholesterol Myth”, the vast majority of cholesterol is produced in the body, primarily by the liver. Although it is portrayed as “bad cholesterol”, LDL (Low Density Lipoprotein) is not really cholesterol but rather a combination of a fat and a protein that carries cholesterol and fats in the bloodstream. High amounts of LDL are not produced without good reason. Merely lowering cholesterol numbers without dealing with why the levels increased in the first place does little to prevent or reverse heart disease.
the liver. Although it is portrayed as “bad cholesterol”, LDL (Low Density Lipoprotein) is not really cholesterol but rather a combination of a fat and a protein that carries cholesterol and fats in the bloodstream. High amounts of LDL are not produced without good reason. Merely lowering cholesterol numbers without dealing with why the levels increased in the first place does little to prevent or reverse heart disease.
The latest research shows that extra cholesterol is sent as a protective mechanism of the body to repair free radical damage in the lining of the coronary artery walls caused by inflammation. The true risk factors of heart disease are those that contribute to the presence of chronic inflammation. When the causes of inflammation are addressed, cholesterol levels easily fall within healthy ranges.
 Inflammation is a normal response of the body to injury. It sets off a number of processes in the body designed to heal the injury. White blood cells and various chemicals are sent to the scene, blood vessels constrict, blood becomes thicker so it can clot and a protective scar forms as cells multiply to repair the damage. For more information on the processes involved in inflammation, I would refer you to my article “Inflammation, the Flame that Fuels the Fire of Disease”
Inflammation is a normal response of the body to injury. It sets off a number of processes in the body designed to heal the injury. White blood cells and various chemicals are sent to the scene, blood vessels constrict, blood becomes thicker so it can clot and a protective scar forms as cells multiply to repair the damage. For more information on the processes involved in inflammation, I would refer you to my article “Inflammation, the Flame that Fuels the Fire of Disease”
When injuries occur repeatedly, inflammation becomes chronic and the healing process is never completed. The “scar” that forms from repeated damage to coronary arteries contributes to atherosclerosis (a condition in which arteries are narrowed from plaque build-up and artery walls thicken). Add to that process the thickening of blood and constriction of blood vessels which occur as part of the inflammatory response, and it is easy to see how blood clots could form to block the flow of blood and cause a heart attack or stroke. Infla
mmation is truly the match that lights the fire of heart disease.
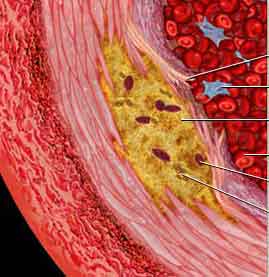
What Contributes to Clogged Arteries
Of greater concern than total cholesterol is the amount and size of LDL particles. The smaller dense particles of LDL more easily turn rancid due to the process of oxidation. Oxidative damage takes place from free radical activity that occurs when anti-oxidant levels are not sufficient enough to deal with the amount of free radicals. The smaller particles of LDL are far more vulnerable to oxidation. Unlike the normal large and “fluffy” particles that harmlessly bounce off arteries like beach balls, these small dense LDL particles easily penetrate and inflict damage as if they were tiny BB pellets. As they imbed in the lining of the arteries, they produce a constant source of irritation or injury that triggers the development of chronic inflammation.
When the cells that line the walls of arteries are damaged, lesions form and underlying collagen is exposed. This creates a “sticky” surface, in which blood platelets adhere as they attempt to cover the lesion to prevent bleeding. Clots form in the arterial wall as a result. The sticky surface created also attracts particles of oxidized cholesterol (which also is “sticky”), calc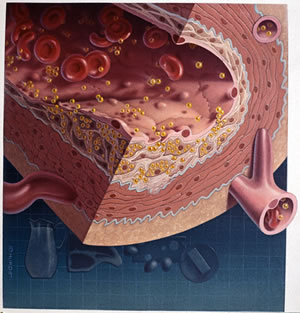 ium and other minerals, all of which
ium and other minerals, all of which
collect in the area. At the same time, the body responds to the inflammatory damage that occurs in the artery walls by signaling the liver to produce and send additional cholesterol to “patch” the afflicted area. Over time, the build-up of plaque from LDL cholesterol and blood clot formation causes arteries to become congested, which increases the risk of a heart attack or stroke.
I hope that you now can better understand that it is not just elevated amounts of “bad” LDL that lead to heart disease but rather the fact that a harmful form of LDL increases according to the amount of damage brought on by oxidation and inflammation. Cholesterol is just doing its job to repair the lesion (remember, cholesterol is needed for the production of new healthy cells) and prevent further damage.
What Do the Numbers Really Mean?
 As I pointed out in last month’s article, a person’s total cholesterol number alone tells very little about their true risk for heart disease (unless it is well over 300). However, the individual numbers and their relationship to each other are significant in revealing underlying causes and risk factors for cardiovascular disease.
As I pointed out in last month’s article, a person’s total cholesterol number alone tells very little about their true risk for heart disease (unless it is well over 300). However, the individual numbers and their relationship to each other are significant in revealing underlying causes and risk factors for cardiovascular disease.
We already established that LDL is sent from the liver to the coronary arteries and may contribute to the formation of arterial plaque in its oxidized state. One of the functions of HDL (High Density Lipoprotein) is to scour the walls of blood vessels and pick up excess cholesterol in the blood, which it then transports back to the liver to either be processed for redistribution or eliminated. HDL is considered the “good cholesterol” since it serves to clear out excess LDL before it becomes harmful. HDL levels over 60 are considered healthy. Ideally, the ratio obtained by dividing total cholesterol by HDL and multiplying that number by 100 should be 25% or above.
When blood cholesterol is tested, two other lipid levels are generally included – triglycerides and VLDL (Very Low Density Lipoprotein). Triglycerides are a form of fat created when the amount of sugar and refined carbohydrates (which convert to glucose in the body) exceed what the body can utilize. The excess is turned into triglycerides for storage in fat cells. Triglyceride levels over 100 are considered a risk factor for heart disease. VLDL is metabolized in the bloodstream to produce LDL. VLDL values indicate the rate at which cholesterol is oxidizing. Higher levels of VLDL (over 10) are a more significant risk factor than even high LDL levels. The lower the VLDL, the better off you are.
The ratio that most reveals the major underlying cause for inflammation leading to arterial damage is the number that results from dividing total triglyceride levels by HDL. If the answer to that calculation is three or greater, you definitely need to pay attention to the following section of this article.
It’s Not the Fat but the Sugar
Most everyone thinks too much dietary fat is what causes cholesterol levels to rise and form plaque deposits. However, low fat diets can actually increase cholesterol levels in the blood. If you remember from last month’s article, 60-80% of the cholesterol produced in the body is used to make bile salts to digest fats. Consuming fats turns more cholesterol into bile salts for digestion, which actually helps to lower cholesterol levels (please understand that I am not endorsing eating unhealthy fats such as trans fats or hydrogenated oils).
So if fat is not the main perpetrator that triggers inflammation and spurs the formation of the harmful form of LDL, what is? Sugar…, along with too many refined carbohydrates which convert to sugar (glucose) in the body. Eating sugar, refined grains and other high glycemic carbohydrates cause blood glucose levels to rise, which triggers the release of insulin by the pancreas. Insulin’s job is to get the glucose out of the bl ood and into the cell to be used for energy production. The more sugar and refined carbohydrates are consumed, the more glucose levels rise and the more insulin is required to bring those levels down.
ood and into the cell to be used for energy production. The more sugar and refined carbohydrates are consumed, the more glucose levels rise and the more insulin is required to bring those levels down.
Over time, repeated spikes in blood sugar and the presence of too much insulin in the blood damages insulin receptors on the cell membranes, which leads to the development of insulin resistance. Once this happens, cells lose their sensitivity to insulin which means greater and greater amounts of insulin are required to escort glucose into the cells. This results in elevated levels of both glucose and insulin remaining in the blood far too long, which creates inflammatory damage in arteries and elsewhere in the body.
The condition of high levels of insulin in the blood is known as hyperinsulinemia. If a person’s total triglyceride number divided by their HDL number is greater than three, hyperinsulinemia is likely present. The higher the ratio between triglyceride and HDL levels, the greater the amount of harmful LDL. The more oxidized LDL, the greater the risk of heart disease, regardless of total cholesterol levels. According to the latest research, high levels of insulin in the blood are a far better predictor of the risk of cardiovascular disease than high cholesterol levels.
Additional Factors Linked to Inflammation
A number of other factors play into the creation of inflammation that contributes to the development of heart disease. The first two are considered markers that indicate the presence of inflammation. Although blood tests that include these two inflammatory markers are not performed as routinely as cholesterol blood tests, they are actually far more revealing than cholesterol numbers when it comes to predicting the true risks for coronary heart disease.
C-Reactive Protein
CRP (C-reactive protein) is a protein substance manufactured in the liver that shows up in the blood in response to chronic inflammation. According to recent studies, risks of heart attacks are tripled in men with high levels of CRP. Elevated CRP levels in women are thought to increase the risk of a heart attack as much as seven times. In an eight-year study that involved 28,000 women, the women with higher levels of CRP were more than twice as likely to have a heart attack as women who had high LDL levels. The relatively small measure of success of statin drugs in lowering incidences of heart disease may be attributed more to their ability to somewhat lower CRP levels rather than their ability to reduce cholesterol levels (although far safer natural ways exist to lower inflammation in the body).
A CRP screening test is valuable in showing the presence of chronic inflammation and the need to lower it in order to naturally decrease the risk of heart disease. A CRP level less than one milligram per liter of blood means a low risk for cardiovascular disease. Between one and three indicates an intermediate risk and over three would indicate a high risk.
Homocysteine
High levels of homocysteine in the blood increase the stickiness of platelets, which adds to the likelihood that clots will develop. It also contributes to oxidized cholesterol, hardening of the arteries and plaque formation. Homocysteine is an amino acid created from the incomplete breakdown of methionine (another amino acid) during protein digestion. Excess amounts can occur if too much meat or other types of animal protein are consumed when a deficiency exists of certain B vitamins (B-6, B-12, folic acid and riboflavin) needed to prevent the conversion of methionine to homocysteine. Studies have shown that people with the lowest levels of these vitamins had the highest death rates from cardiovascular disease and heart attack. Increasing dietary sources and supplements containing these B vitamins blocks the conversion of methionine to homocysteine.
Exposure to Toxins
Increased amounts of chemicals and other toxins in our modern society may also play a significant role in creating elevated cholesterol levels. The body produces extra amounts of cholesterol to engulf and bind these fat-soluble toxins and heavy metals in order to protect the nerves and brain from exposure to them until they can be safely eliminated from the body. Because toxins irritate tissues and cause free radical damage, the body is once again responding to inflammatory damage and using cholesterol to protect itself from further exposure and damage. Lowering cholesterol levels with drugs without taking action to remove the inflammation-producing toxins means less cholesterol is available to bind to them. This puts the health of the body in jeopardy by allowing inflammatory damage to increase, which in turn, increases the risk factors that lead to the development of cardiovascular disease.
Excess Amounts of Omega-6 Fatty Acids
The right balance of essential fatty acids is vital for metabolizing cholesterol, co ntrolling insulin and reducing inflammation. As I explained in my article “Understanding Fats – The Good, the Bad and the Best – Part 2”, the ratio between the amount of foods high in omega-6 fatty acids and foods high in omega-3 fatty acids is extremely imbalanced in the diets of most Americans due to the widespread use of polyunsaturated vegetable oils (the average person consumes 20-25 times more omega-6 fatty acids than omega-3).
ntrolling insulin and reducing inflammation. As I explained in my article “Understanding Fats – The Good, the Bad and the Best – Part 2”, the ratio between the amount of foods high in omega-6 fatty acids and foods high in omega-3 fatty acids is extremely imbalanced in the diets of most Americans due to the widespread use of polyunsaturated vegetable oils (the average person consumes 20-25 times more omega-6 fatty acids than omega-3).
The problem is that linoleic acid (the primary fatty acid found in vegetable oil) converts to arachidonic acid, which then is converted by special enzymes to inflammatory producing substances (prostaglandin P2 and interleukin cytokines). These inflammatory molecules promote inflammation in arterial walls as well as throughout the entire body. On the contrary, the right omega-3:omega-6 ratio promotes the type of chemical messengers that reduce inflammation, dilate blood vessels, prevent platelet aggregation (clotting of blood) and lower arterial pressure.
High Acid Diet
The muscle tissue in arterial walls can be irritated, inflamed and scarred from high levels of lactic acid, when it is not sufficiently cleared from the body. The typical American diet is far too high in meats, sugar, grain, starch and other acidifying foods and too low in alkaline foods such as fresh fruits and vegetables (for more information on how to obtain the right pH balance in your diet, I would refer you to “Understanding pH – Your Health is in the Balance – Part 2”.
Practical Steps to Reduce Inflammation and Heart Disease
What are the best ways to reduce the risk of heart disease? It so happens that the factors that cause imbalances in the body which place us at risk for cardiovascular disease – diet, nutritional intake, exercise, stress levels, - are all factors within our ability to control. Even if people are genetically predisposed to heart disease, choices involving diet and lifestyle choices ultimately determine their outcome.
FACTORS RELATED TO DIET
Following the dietary guidelines listed below will not only help reduce your risk of cardiovascular disease but will also help you lose excess weight and increase your level of health in every area.
General Dietary Guidelines
-
Increase consumption of whole foods rich in phytonutrients (plant molecules) that give the body the nutrients it needs. Eat good amounts (seven to nine servings are recommended) of fresh fruits and vegetables and/or supplement to provide your body with the vitamins, minerals, anti-oxidants, anti-inflammatory molecules and other phytonutrients that can reverse inflammation and heal damaged tissues.
-
Drink plenty of pure water – lack of sufficient hydration thickens the blood, increases blood pressure and contributes to hardening of the artery walls. A sufficient intake of water keeps the blood thinner, blood pressure regulated, artery walls more supple, in addition to flushing out harmful forms of excess cholesterol.Drink at least one half an ounce for every pound of body
 weight daily.
weight daily. -
Increase soluble fiber in dietary or supplemental form as it mops up oxidized cholesterol in the bile from the liver before it can be reabsorbed. Eat enough high-fiber beans, whole grains, vegetables, nuts (raw, not roasted), seeds and fruit to take in 35-50 grams of fiber per day. To make up for shortfalls in the diet, include a good natural fiber supplement as part of your daily routine.
-
Avoid dietary forms of oxidized cholesterol (cholesterol that has gone rancid) from the consumption of overcooked proteins such as meats and eggs (to prevent the oxidation of cholesterol in eggs, eat them lightly cooked with the yolks intact).
- Do not avoid eggs thinking they are too high in cholesterol. A study based on 117,000 people that was published in the Journal of American Medical Association showed that those who ate the most eggs (six per week or more) had the lowest risk of heart attacks whereas the group that ate the fewest eggs (less than one per week) actually had the highest incidences of heart attacks. Eggs are an excellent source of protein and other nutrients to build muscle, tissues and cell membranes plus they contain folic acid, which helps to control homocysteine levels. Eat eggs from free-range chickens (organic, omega-3 fed if possible).
Control Blood Sugar Levels 
-
Eliminate (or at least greatly reduce) your intake of refined sugars and grains.
-
Eat mostly low glycemic carbohydrates that don’t trigger high levels of insulin (non-sugary fruits and all non-starchy vegetables).
-
Eat protein with every meal and snack. It is especially important to have a good protein breakfast every day. Never eat carbohydrates alone (try to combine protein, fat and carbohydrates in every meal and snack).
- Eat every few hours to keep blood sugar levels from dropping (low blood sugar produces hunger and cravings which may tempt you to indulge in refined carbohydrates or overeat).
- Drink plenty of pure water; avoiding sodas,juices, and diet drinks that impact sugar and fat metabolism (liquid sugar calories are the biggest contributors to obesity and diabetes and heart disease – high fructose corn syrup is more to blame than any other form of sugar).
-
Avoid or reduce alcohol, which can increase triglycerides and fat in the liver and create blood sugar imbalances.
Eat the Right Fats
-
Avoid eating low-fat diet products which usually contain added sugars.
- Avoid all forms of trans fats. This means anything with hydrogenated or partially hydrogenated oils (read labels of processed foods carefully!), including margarine, commercial baked goods (the bromide that replaced iodine as a dough conditioner in commercial baked goods interferes with fat metabolism), restaurant fried foods, etc. Trans fats increase LDL, reduce HDL and interfere with the normal metabolism of omega-3 fats and the function of cell membranes that affects cellular communication. The heart runs on fats and needs good fats to be healthy.

-
Greatly reduce the use of refined vegetable oils (corn, soybean, sunflower, cottonseed, safflower, canola and other vegetable oils) and the processed foods that contain them.
-
Change the oil when it comes to your diet - use healthy oils like extra virgin olive oil, cold-pressed sesame oil, nut oils, extra virgin coconut oil and organically produced butter or ghee Both coconut oil, butter and ghee contain medium chained saturated fats that are beneficial to the heart and body (see my articles on “Healthy Cooking Oils” for more information).
-
Eat more omega-3 food sources such as wild salmon, avocados, dark green, leafy vegetables, walnuts, hemp, pumpkin or flax seeds. (Freshly ground flax seeds can be used in shakes, or sprinkled on salads or whole grain cereal).
- Limit amounts of saturated fats from animal sources that are not grain-fed as those fats are more saturated and contain toxins that reside in the fat of commercially produced beef (see my article “True Facts on Fat” for more information on this subject).
-
Add CLA (conjugated linoleic acid) to your diet from grass-fed dairy products and meat. CLA is known to increase energy, improve insulin sensitivity, reduce abdominal fat and preserve muscle mass. It also acts to increase anti-inflammatory prostaglandins and reduce pro-inflammatory ones at the same time (CLA is also available in supplement form).
LIFESTYLE FACTORS
Lose Weight - Being overweight (especially weight in the abdomen area) contributes to inflammation as fat cells at a certain stage begin to produce inflammatory molecules. Since more blood vessels are created to supply surplus fat tissue, the heart is placed under added strain, as it has to pump blood through an additional mile of blood vessels for every extra pound of fat. Losing weight helps to decrease levels of blood fats and LDL in addition to raising HDL levels. For help with healthy weight loss, I would refer you to my series on “Health-Gain Weight-Loss”.
healthy weight loss, I would refer you to my series on “Health-Gain Weight-Loss”.
Reduce and/or Manage Stress – Raised levels of stress hormones affects blood sugar levels and contributes to inflammation. Continued release of stress hormones eventually exhausts the adrenal glands, which results in suboptimal hormone production. Cholesterol levels rise in response to the body’s need to produce adrenal hormones since cholesterol is a precursor to hormone production. Stress can also cause blood pressure to rise and adversely affects blood clotting.
Exercise – The heart is a muscle and exercise is required to build muscle strength. Exercise increases oxygen levels and blood flow to the coronary arteries in addition to lowering stress levels.
Stop Smoking – Smoking decreases oxygen levels to the heart and other tissues, damages cells that line coronary arteries and lower HDL levels.
ADDITIONAL MEASURES
Minimize Exposure to Environmental Toxins - Avoid toxic chemicals like chlorine, bromides, solvents, heavy metals, pesticides, etc. For more information on reducing levels of toxins in your diet and surroundings, please read my article “Detoxifying for Better Health – Part 5”.
Optimize Liver Function – Since the liver is the prime producer and distributor of cholesterol, a healthy liver is important for managing cholesterol levels in the body. Periodically cleansing the liver helps to flush accumulated fats and cholesterol from both the liver and gallbladder. It also keeps receptors on the surface of liver cells responsible for removing LDL from the blood flushed to make room for new “deposits”. LDL levels lower when it is removed from the blood more quickly.
SUPPLEMENTS TO SUPPORT HEART HEALTH
Though by no means inclusive, listed below are brief descriptions of some of the most important nutrients and herbs for heart health that can be taken in supplement form when dietary amounts are insufficient.
Vitamins, Minerals and Anti-oxidants
-
Vitamin C – important for counteracting free radical damage and facilitating the repair of arteries when they are damaged, thereby preventing the deposit of plaque at the site of injury. Vitamin C also strengthens and restores the elasticity of the blood vessels and elevates levels of HDL.
-
Vitamin E – considered the most active anti-oxidant and fat-soluble vitamin of the cardiovascular system. Studies show that Vitamin E supplementation significantly reduces risk of heart attack by as much as 70%. Vitamin E prevents the oxidation of cholesterol and acts as a natural blood thinner by inhibiting blood coagulation, which helps to prevent blood clots. It also enables the body to utilize oxygen more efficiently at the cellular level. (Avoid vitamin E products that say “dl” alpha tocopherol as they are synthetically produced from substances with an opposite molecular spin than that of the bodies. A truly natural vitamin E that the body can utilize will only say “d” alpha tocopherol).
-
Co-Q10 – helps with energy production in the heart muscle, acts as an anti-oxidant to scavenge free radicals and inhibits oxidative damage to cell membranes and LDL. Co-Q10 also regenerates other antioxidants (such as vitamin E), and stimulates cell growth.
-
Magnesium – is mineral that is a natural relaxer. It helps heart and blood vessels to relax properly, which reduces stress on the heart and protects it against spasms.
Omega-3 Fatty Acids –
-
Fish Oil – mounting evidence shows that omega-3 fatty acids from fish oil supplements helps prevent cardiovascular diseases in healthy individuals in addition to reducing incidences of cardiac events in heart disease patients. Patients who consume the most omega-3 had a 55% lower risk of death from cardiovascular disease, heart attack, death and stroke and a 51% less risk of death from coronary artery disease and every other disease was less as well. Taking 1,000 mg. a day reduced the likelihood of sudden death through heart disease by 45%. Omega-3 fatty acids are powerful natural anti-inflammatory agents that help to thin the blood and prevent blood coagulation in addition to reducing blood fats and LDL levels.
-
Krill Oil – is an extremely bioavailable source of omega-3 fatty acids as well as a natural source of astaxanthin, which is a powerful antioxidant carotenoid. Krill oil naturally contains phospholipids that bind to omega-3 fatty acids and improve their absorption in the body. Krill oil helps to lower blood fat, blood sugar and LDL levels even more effectively than fish oil.
-
Flaxseed Oil - a nutritious oil that provides a vegetarian source of omega-3 as well as beneficial forms of omega-6 fatty acids. Flaxseed oil helps lower cholesterol levels.
Herbs
-
Hawthorn Berry– is considered the herb of the heart. It works to nourish and strengthen the heart by dilating blood vessels so it gets more blood and does not have to pump as hard to get blood to the extremities. It also helps to strengthen and normalize heart rhythm.
-
Capsicum – is considered the herb of the entire circulatory system. It increases circulation, strengthens the heartbeat and helps break down cholesterol and convert it into bile acids so it can be excreted out of the body.
- Garlic – acts like a blood thinner to inhibit the clumping of blood cells (platelet aggregation), helps to break down and lessen the production of fibrinogen. Garlic also helps breakdown triglycerides and reduces blood fat as well as raise levels of HDL. Additionally, it helps to decrease circulating blood glucose and improve insulin sensitivity.
-
Olive Leaf - anti-oxidant compounds contained in this herb help to inhibit the oxidation of LDL and reduce the aggregation of blood platelets on inflamed arterial walls. It is also considered helpful to lower blood pressure and normalize heart beat irregularities.
-
Ginkgo – acts as a vasodilator to open constricted blood vessels, enhancing blood flow to the heart muscle as well as the brain. Ginkgo also helps to reduce inflammation and platelet accumulation and increase peripheral circulation.
Concluding Thoughts
Most heart disease develops as a result of factors related to diet and lifestyle. Fortunately, using means that naturally support the heart and the entire cardiovascular system can help to reverse it. Unlike drugs that often produce harmful side effects, natural substances give the body what it needs to heal itself. By daily choosing to eliminate the factors that lead to inflammation and oxidative damage in the body, we can effectively reduce the underlying causes of heart disease and improve our overall health in the process.
Sources:
Ultra Prevention – by Mark Hyman, M.D. and Mark Liponis, M.D.
You Don’t Have to Die of a Heart Attack! By Gerald M. Lemole, M.D.
Cholesterol and Your Health –Separating Fact From Fallacy by Kimberly Balas, ND, Ph.D. and Steven H. Horne, RH(AHG)
http://articles.mercola.com/sites/articles/archive/2008/12/06/6-ways-to-reduce-inflammation-without-a-statin-drug.aspx
http://drhyman.com/lower-your-risk-of-heart-disease-without-drugs-575/
HEART SUPPLEMENTS AND FORMULAS TO CONSIDER
If you are interested in taking quality supplements to effectively support heart health, I would recommend that you read the research documents on those I have listed below. Many of these supplements contain a combination of several nutrients that are specially formulated to enhance the heart and circulatory system.
Super Omega-3: a pure pharmaceutical grade fish oil stabilized with lemon oil. It contains both EPA and DHA omega-3 fatty acids.
Krill Oil: contains krill, fish oil and vitamin K
Flaxseed Oil with Lignans
Ginkgo Hawthorn Combination: a combination of ginkgo, hawthorn and olive leaf used to support increased blood circulation and oxygen throughout the body. It provides enhanced oxygen utilization in the heart muscle and helps prevent blood clots from forming.
HS II: a combination containing capsicum, garlic, and hawthorn that works to stimulate coronary blood flow and strengthen weaknesses in the circulatory system.
Cardio Assuance: a blend of nutrients (B6, B12, folic Acid, K2, hawthorn berries, and reseratrol), which help to metabolize homocysteine and provide anti-oxidant protection for the heart.
Capsicum, Garlic and Parsley: a combination of three herbs know to support circulation and help regulate blood pressure and cholesterol levels.
Mega Chel: a powerful oral chelation formula that can be used to help reverse arterial plaque buildup and improve circulation to heart and other areas of the body.
Guggul Lipid: an herb used in Ayurvedic medicine known to lower triglyceride and LDL levels and raised HDL levels.
Red Yeast Rice: used for centuries as a medicinal food for improving blood circulation. It helps to normalize the body’s cholesterol production by increasing the liver’s removal of LDL. CoQ10 supplementation should accompany the use of this substance.
CoQ10
Garlic
Capsicum
Hawthorn Berries
Cardio Assuance: a blend of nutrients (B6, B12, folic Acid, K2, hawthorn berries, and reseratrol), which help to metabolize homocysteine and provide anti-oxidant protection for the heart.
Copyright © 2008-2015 Lucinda Bedogne, CNHP, CNC
Post Your Comment...
|
|
||||||||||||



